- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
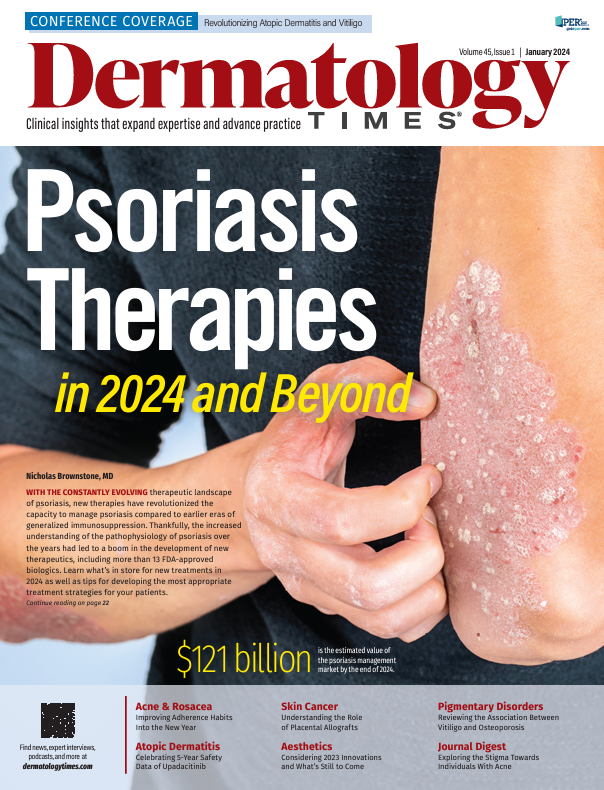
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
News
Article
Dermatology Times
Silver Linings With the Silverbergs: Showcasing Vitiligo and Atopic Dermatitis Research
Author(s):
Innovative practice pearls for both vitiligo and atopic dermatitis treatment were shared with nearly 200 clinicians to put into practice at the virtual Revolutionizing Vitiligo and Revolutionizing Atopic Dermatitis Conferences.
Nanette Silverberg, MD, chief of pediatric dermatology at Mount Sinai Health System in New York, New York, and Jonathan Silverberg, MD, PhD, MPH, associate professor of dermatology and director of clinical research and contact dermatitis at the George Washington University School of Medicine and Health Sciences in Washington, DC, joined forces to host the virtual Revolutionizing Vitiligo and Revolutionizing Atopic Dermatitis Conferences online in December. Innovative practice pearls for both vitiligo and atopic dermatitis (AD) treatment were shared with nearly 200 clinicians to put into practice. Here are a few highlights.
Study Results Find Association Between Vitiligo and Osteoporosis
Vitiligo and osteoporosis share an association with one another, according to a poster.1
A retrospective cohort study used data from a health services database in Israel called Clalit Health Services. Data were collected from 2002 to 2018.
The study involved a control group wherein patients with vitiligo were matched by age, sex, body mass index, smoking status, and ethnicity. The analysis involved approximately 20,000 patients with vitiligo and nearly 99,000 otherwise healthy patients for the control group.
On average, the age of patients was approximately 33 years, with 51% of participants being female patients. Additionally, 72% of patients were Jewish.
During the follow-up time (a total of 110,000 person-years), researchers noted 284 new onset cases of osteoporosis among patients with vitiligo, with 1185 new onset cases reported among the control group. This was indicative of a higher incidence rate (2.6 cases per 1000 person-years) vs that of the control group (2.2 cases per 1000 person-years).
According to the study findings, the main predictors of osteoporosis in patients with vitiligo included age at onset of vitiligo, female sex, Jewish ethnicity, hyperlipidemia, and obesity. “Dermatologists and primary care physicians should be aware of this association,” said study author and presenter Naama Cohen. “Further epidemiological studies are needed to validate our results.”
Upadacitinib for Vitiligo Improves Patient Health-Related QoL After 24 Weeks
Upadacitinib 22 mg may improve patient-reported health-related quality of life (HRQoL) in adult patients with nonsegmental vitiligo, according to a Revolutionizing Vitiligo Conference poster.2
In the 52-week, phase 2, multicenter, randomized, double-blind, placebo-controlled, dose-ranging study (NCT04927975), adult patients aged 18 to 65 years with nonsegmental vitiligo and a Facial Vitiligo Area Scoring Index score of 0.5 or more and a Total Vitiligo Area Scoring Index score of 5 or more at baseline were included. During a 24-week, double-blind, placebo-controlled treatment period, patients were randomly assigned to receive upadacitinib 6 mg (UPA6), upadacitinib 11 mg (UPA11), upadacitinib 22 mg (UPA22), or placebo once daily.
In total, 185 patients were enrolled in the study (UPA6 n = 49; UPA11 n = 47; UPA22 n = 43; placebo n = 46). Mean reductions in vitiligo QoL scores from baseline to week 24 with UPA22 (−6.6) and UPA6 (−7.5) were numerically larger than with placebo (−5.5) although not statistically significant. At week 24, more patients treated with UPA22 reported a VNS response of “a lot less noticeable” or “no longer noticeable” than with placebo (11.6% vs 0%, respectively; P < .05). “These initial findings suggest that UPA22 may improve patient HRQoL and perceptions of vitiligo noticeability; longer-term data from the extension phase of this study will further clarify the impact of UPA treatment on QoL,” the study authors concluded.
A Link Between Atopic Dermatitis and Altered Oral Microbiome
An association between atopic dermatitis (AD) and an altered oral microbiome/oral dysbiosis was explored in a recent study, as presented in a poster.3
The study, which involved 45 participants with AD and 41 patients without AD matched for age and sex, assessed various oral health indicators. Samples of oral flora were collected and subjected to high-throughput 16S rRNA gene sequencing analysis for microbiome assessment.
Despite no significant differences in demographic and clinical characteristics between the 2 groups, participants with AD exhibited significantly poorer plaque and oral hygiene indices. There was also a noticeable trend toward a higher gingival index in the AD group. Furthermore, the oral microbial diversity in the AD group was found to be significantly higher compared with that of the control group.
The Faith phylogenetic diversity test indicated increased oral microbial diversity in patients with AD, and the analysis of β-diversity demonstrated distinct clustering of microbial communities between patients with AD and patients in the control group. This dissimilarity was statistically significant and suggested an association between AD and altered oral microbiota. Furthermore, patients with AD exhibited a significant increase in the abundance of taxa correlated with oral diseases, whereas there was a decreased abundance of bacteria associated with oral health.
Findings From Largest Safety Study on Upadacitinib Show Promising Long-Term Results in AD Management
Christopher Bunick, MD, PhD, associate professor of dermatology and physician-scientist at the Yale School of Medicine in New Haven, Connecticut, presented a late-breaking research session on 5-year safety data on upadacitinib (Rinvoq) in 15-mg and 30-mg doses, integrating information from 3 global phase 3 studies: Measure Up 1 (NCT03569293), Measure Up 2 (NCT03607422), and AD Up (NCT03568318). The study looked at approximately 2700 patients and featured an extended 260-week follow-up, making it the longest safety investigation for any systemic atopic dermatitis (AD) agent.
Key findings included an increased rate of eczema herpeticum observed with upadacitinib 30 mg vs 15 mg in the 5-year analysis, with a dose-dependent increase in herpes zoster. There were slightly higher rates of serious infections and opportunistic infections observed with upadacitinib 30 mg vs 15 mg. No dose relationship was observed for nonmelanoma skin cancer (NMSC) and malignant tumor excluding NMSC. Rates of adjudicated major adverse cardiovascular events (MACEs) and adjudicated venous thromboembolic events (VTEs) were low (≤ 0.2 E/100 PY). The reporting of MACEs, VTEs, and malignant tumors (excluding NMSC) in the upadacitinib phase 3 clinical trials for AD generally reflects the background observations of these events in the population with AD. The conclusion supports the confident consideration of prescribing upadacitinib for patients with AD.4
References
- Cohen N. Vitiligo is associated with new onset osteoporosis: a population-based study. Presented at: 2023 Revolutionizing Vitiligo Virtual Conference; December 10, 2023.
- Ezzedine K, Soliman A, Rosmarin D, Pandya A, Schlosser BJ, Geel N. Patient-reported outcomes following 24 weeks of treatment with upadacitinib in adults with non-segmental vitiligo: results from a phase 2, randomized, double-blind, dose-ranging study. Poster presented at: 2023 Revolutionizing Vitiligo Virtual Conference; December 10, 2023.
- Shahin A, Leshem YA, Taieb Y, et al. Adult atopic dermatitis is associated with impaired oral health and oral dysbiosis- a case-control study. Poster presented at: 2023 Revolutionizing Atopic Dermatitis Virtual Conference; December 10, 2023.
- Bunick C. Long-term 5-year safety of upadacitinib in moderate-to-severe atopic dermatitis: an integrated analysis including over 7000 patient-years of exposure. Presented at: 2023 Revolutionizing Atopic Dermatitis Virtual Conference; December 10, 2023.