- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
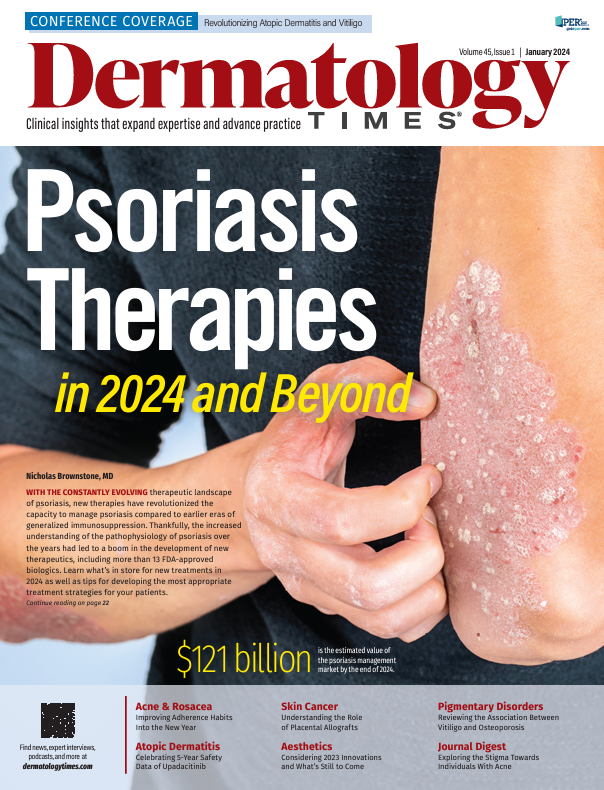
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Consider PDE4 Inhibitors for Mild to Moderate Psoriasis
Author(s):
Lisa Swanson, MD, FAAD, and Robert Casquejo, PA-C, discuss their preferred treatment approach for plaque psoriasis, which includes PDE4 inhibitors such as apremilast and roflumilast.

“It’s so easy when you encounter a patient with severe plaque psoriasis to empathize and understand the impact it’s having on their life when they’re virtually covered in psoriasis. But I think a lot of people under underestimate the impact of mild psoriasis on a person experiencing it, especially given where on their body it’s affecting,” said Lisa Swanson, MD, FAAD, during a custom Dermatology Times DermView video series, “Unveiling the Potential of PDE4 Inhibitors: Expanding Horizons Beyond Topicals in Plaque Psoriasis.” Swanson, a board-certified pediatric dermatologist at Ada West Dermatology in Boise, Idaho, was joined by Robert Casquejo, PA-C, a board-certified physician assistant and the CEO of Skin and Cancer Center of Scottsdale in Arizona, to discuss their treatment approach for plaque psoriasis.
Topical Therapy Limitations Due to Body Location
To kick off their discussion, Swanson and Casquejo agreed that topical management of psoriasis, specifically on the scalp, can be challenging. To begin creating his treatment strategy, Casquejo asks his patients how physically bothered they are by their scalp psoriasis. The top complaint he hears from patients is itch that affects their daily activities and sleep, which is worrisome for many patients. To assess the psychosocial impact, Casquejo then asks his patients how badly they want to get rid of their psoriasis.
“It’s an open-ended enough question that you’ll get someone to tell you, ‘It’s the worst thing that’s ever happened to me.’ And then that should set your expectations and your role as the provider,” said Casquejo.
Swanson mentioned that many of her patients are not completely satisfied with currently available topical therapies for scalp psoriasis treatment, citing concerns with oiliness of their hair after application.
“With patients with areas of involvement like the scalp, sometimes I move a little bit more quickly to a systemic treatment option, just because of ease of use,” said Swanson.
Discussing Systemic Therapies for Patients
“I’m almost into the systemics right out of the gate, and this is from a person who likes phototherapy...but I’m going to start thinking ahead to these more aggressive treatments based on not only what I see in severity but also how the patient feels about it,” said Casquejo.
Swanson discussed that as dermatology clinicians’ knowledge and understanding of psoriasis as a systemic inflammatory process has improved over the years, the “desire to treat it systemically has definitely increased.”Most importantly to Swanson, there are many comorbidities associated with psoriasis, and by treating patients systemically, clinicians may help the overall health of their patient.
When starting the systemics discussion with their patients, both Swanson and Casquejofirst collect a detailed patient history that includes a history of breast cancer and solid tumors within the past 5 years or a family history of inflammatory bowel disease. Both clinicians emphasized the importance of asking patients whether they prefer an oral medication or injection.
Choosing PDE4 Inhibitors for Plaque Psoriasis
A phosphodiesterase-4 (PDE4) inhibitor cleaves cyclic adenosine monophosphate (cAMP) to AMP, causing a cascade of proinflammatory mediators. By inhibiting PDE4, the cascade of proinflammatory meditators is inhibited, which is how the class of PDE4 inhibitors such as apremilast (Otezla; Amgen) and roflumilast (Zoryve; Arcutis Biotherapeutics) came to be investigated, according to Swanson. Apremilast is an oral PDE4 inhibitor for patients 18 years or older with plaque psoriasis, whereas roflumilast cream is a topical PDE4 inhibitor for patients 6 years or older.
Casquejo noted that when apremilast was first approved, he was impressed with its narrow adverse effect profile and no boxed warnings compared with Janus kinase (JAK) inhibitors. Casquejo attributes apremilast’s success to its narrow adverse effect profile, its convenience as an oral pill, and no major laboratory work needed compared with JAK inhibitor requirements.
“I found apremilast was a great stepping stone medication because people were now not afraid to try something new,” said Casquejo.
Swanson noted that a few of her patients with psoriasis have complained of diarrhea as an adverse event that prevents them from continuing with apremilast. When asked for his advice, Casquejo discussed how he presents adverse effects to his patients from the start and emphasized that most adverse effects with apremilast, including diarrhea, are treatable.
Apremilast for Mild to Moderate Psoriasis
One of the key points of Swanson and Casquejo’s discussion was the significance of apremilast being approved for mild to moderate psoriasis, not just severe psoriasis. Swanson noted that although dermatology providers do well at discussing and treating severe diseases, there is room for improvement when discussing mild diseases, and in their discussion, mild to moderate psoriasis.
“I see a lot of patients who have mild disease, but it’s chronically hopping around. Sometimes I’ll talk to them about a systemic agent because they feel like they’re playing a game of whack-a-mole. They clear over here, and they’re excited about that, but boom, now it’s over here. So it might be mild, but it’s just playing games with them, and going on a systemic therapy might be appealing,” said Swanson.
Swanson and Casquejo concluded their discussion by discussing future advancements of PDE4 inhibitors and apremilast, and specifically that apremilast is currently being studied for pediatric psoriasis in the phase 3 SPROUT (NCT03701763) study.1
Reference
- Efficacy and safety of apremilast (CC-10004) in pediatric subjects from 6 through 17 years of age with moderate to severe plaque psoriasis. ClinicalTrials.gov. Updated December 7, 2023. Accessed December 12, 2023. https://clinicaltrials.gov/study/NCT03701763