- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Melanoma diagnosis by physician or PA not always straightforward
Author(s):
In a comparison of the performance between physician assistants and dermatologists, physician assistants may have lower diagnostic accuracy for melanoma than dermatologists, suggests a study published in JAMA Dermatology. The AAPA and SDPA question the use of the NNB ratio to determine diagnostic accuracy.
In a comparison of the performance between physician assistants and dermatologists, physician assistants may have lower diagnostic accuracy for melanoma than dermatologists, suggests a study published in JAMA Dermatology.
The article, “Accuracy of Skin Cancer Diagnosis by Physician Assistants Compared with Dermatologists in a Large Health Care System,” published in April, is a medical record review of 33,647 skin cancer screening examinations on 20,270 patients (64.9%) who were treated at a single center between Jan. 1, 2011 – Dec. 31, 2015.
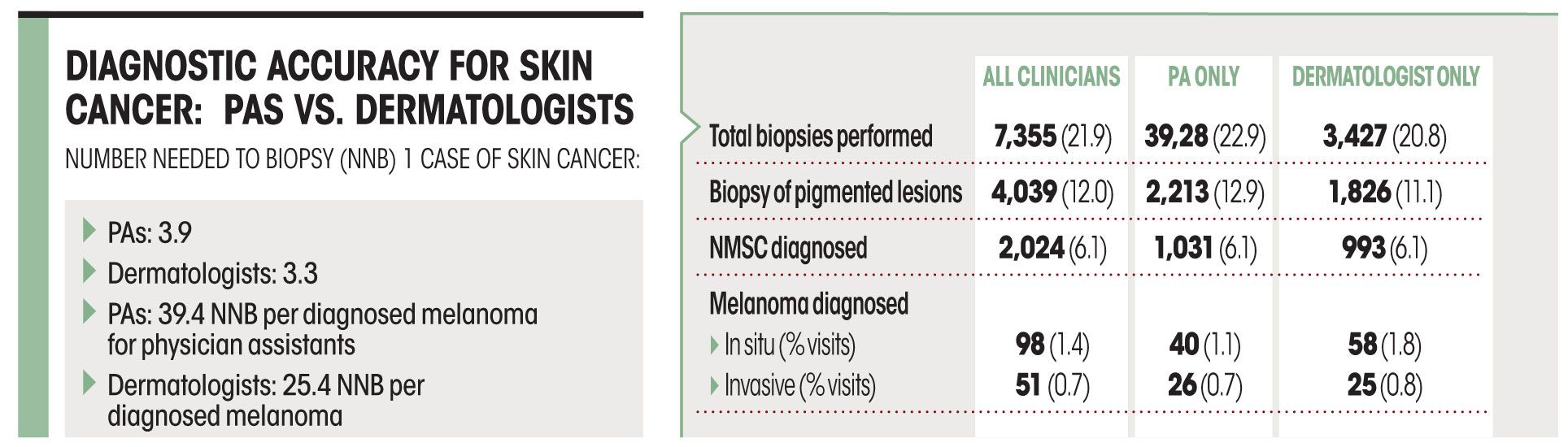
The study found that to diagnose one case of skin cancer, the number needed to biopsy (NNB) was 3.9 (22.9%) for PAs and 3.3 (20.8%) for dermatologists. Per diagnosed melanoma, the NNB was 39.4 for PAs and 25.4 for dermatologists. Screenings performed by dermatologists were more likely to result in a diagnosis of melanoma in situ 1.8% vs. 1.1%, P = .02), but differences were not significant for invasive melanoma or nonmelanoma skin cancer, which is a telling point, according to the American Academy of Physician Assistants (AAPA) and the Society of Dermatology Physician Assistants (SDPA).
The AAPA and SDPA question the use of the NNB ratio to determine diagnostic accuracy. NNB is controversial - even among dermatologists, they stated. In August 2016, Michael A. Marchetti, M.D., et al., wrote in JAMA Dermatology: “Considering NNB without attention to the sensitivity applied to the detection of skin cancer and the prevalence of skin cancer could prove misleading.”
Thirty clinicians (15 dermatologists and 15 PAs) provided skin cancer screening, which in itself is potentially problematic due to the small size, AAPA and SDPA contends. Patients with a history of melanoma were more likely to see a dermatologist, whereas those with a history of any type of skin cancer were more likely to see a physician assistant.
“While the article states that the 15 PAs saw a higher percentage of people with a history of skin cancer, the dermatologists saw more patients with a history of melanoma. We would expect a higher rate of melanoma diagnosis in this patient population. Also, these patients with a history of melanoma could be choosing to see the dermatologist over the PA. In the same vein, people who seek removal of a non-cancerous skin lesion for cosmetic or convenience reasons may choose to see the PA for ease of getting an appointment, rather than the dermatologist,” states the AAPA and SDPA.
“There is no way to fully separate the decision making of the PA from the decision making of the physician because in this case, the physician assistant must have supervisory agreement by a physician.”
The authors of the study, who were led by Laura K. Ferris, M.D., Ph.D. of the University of Pittsburgh wrote:
“Although the availability of PAs may help increase access to care and reduce waiting times for appointments, these findings have important implications for the training, appropriate scope of practice, and supervision of PAs and other non-physician practitioners in dermatology.” “Missed diagnoses or unnecessary biopsies of benign lesions should be factored into decisions about the scope of a practice, hiring decisions, supervision of providers and patient decisions about who provides their dermatologic care,” Dr. Ferris and colleagues wrote.
REFERENCES
Ayce M. Anderson, PhD; Martha Matsumoto, MD; Melissa I. Saul, MS; et al. “Accuracy of skin cancer diagnosis by physician assistants compared with dermatologists in a large health care system,” JAMA Dermatology. April 18, 2018. DOI:10.1001/jamadermatol.2018.0212
Michael A. Marchetti, MD; Stephen W. Dusza, DrPH; Allan C. Halpern, MD. “A Closer Inspection of the Number Needed to Biopsy,” JAMA Dermatology, August 2016. DOI:10.1001/jamadermatol.2016.0936






