- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Head and neck melanoma characteristics
Author(s):
Melanoma located on the head and neck are associated with a potentially worse prognosis relative to alternate anatomical sites and peripherally located melanoma compared to those centrally located.
(Melanoma lavizzara - stock.adobe.com)
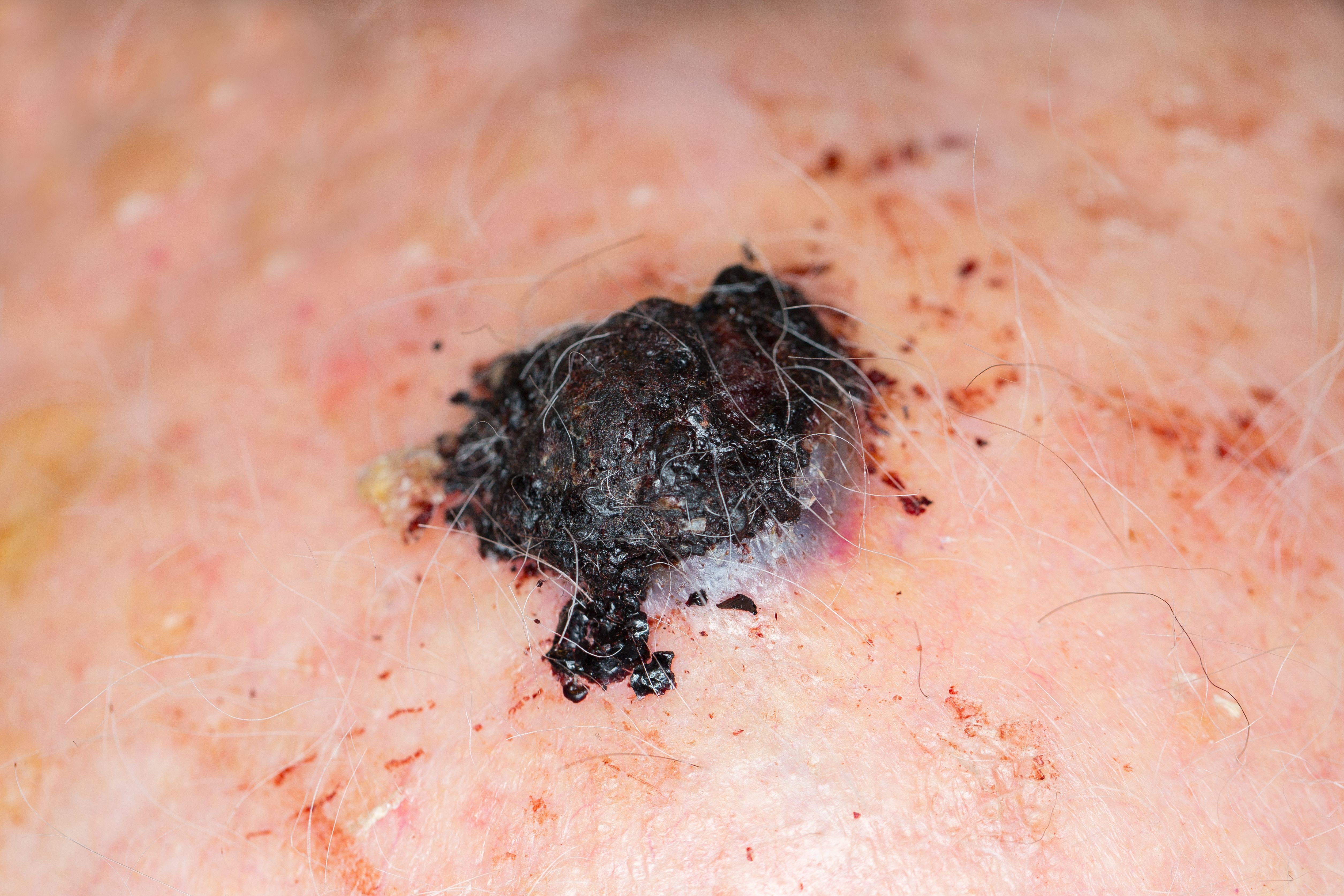
Clinicians should be aware of higher risk cutaneous head and neck melanoma (CHNM) lesions and their potentially worse prognosis when considering appropriate therapies for their patients. According to recent data, CHNM have poorer outcomes relative to melanoma on alternate anatomical sites.1 And, more specifically, peripherally located CHNM appear to have poorer outcomes than centrally located CHNM, a new study indicates.2
Cutaneous head and neck melanomas have distinct characteristics and have been reported to constitute approximately 12% to 21% of melanomas annually. The primary environmental risk factor for the development of melanoma is sun exposure, particularly intermittent and intense exposures in childhood that lead to blistering sunburns. This may, in part, explain the high incidence of melanoma in the head and neck region.
RELATED: Skin cancer imaging device speeds diagnosis
There are several factors that are thought play a role in the poorer outcomes seen in CHNM. Compared with melanomas that occur on other anatomic locations, this subset of tumors may be thicker at the time of diagnosis and may present at a more advanced stage.
In addition, the optimal tumor resection margins in the head and neck region are oftentimes very challenging to achieve due to anatomic constraints. And, lymphatic drainage of this region is variable and complex.
Although epidemiologic and clinical-histological differences according to sublocations (peripheral vs. central) have been reported in the literature, their impact on survival has not been largely explored.
In a recent retrospective study, José Antonio Avilés-Izquierdo, M.D., and fellow colleagues from the department of dermatology, Hospital General Universitario Gregorio Marañón, Madrid, Spain, evaluated the epidemiological, clinical, histological and survival characteristics in a cohort of patients with CHNM.
A total of 371 patients (female: n=191; male: n=180) with a histological diagnosis of CHNM were included in the study and were followed up for a mean of 93.6 months. CHNM were classified according to ultraviolet radiation exposure into peripheral (i.e., scalp, ear and neck) or central (i.e., forehead, eyelids, nose, cheeks, and perioral region) lesions. Researchers found that peripheral melanomas were much more common in men, were diagnosed at a younger age, had deeper tumor thickness, were more frequently ulcerated, and had a higher (≥6) number of mitoses than those melanomas located centrally.
Data also showed that patients with peripherally located melanomas developed more metastasis, had a higher melanoma-specific mortality, as well as a lower 10-year survival rate (50% vs. 90%; p<0.001) than those with centrally located melanomas.
“Cutaneous head and neck melanomas have been associated with poor outcomes, especially those located on the scalp. The reason for this difference, and whether it is applicable to all locations within the head and neck, remains unclear to this date,” wrote José Antonio Avilés-Izquierdo, M.D., Ph.D., Enrique RodrÃguez-Lomba, M.D., and colleagues, in the study to soon be published in The Journal of the American Academy of Dermatology.
RELATED: GEP testing promising in melanoma
Several different factors in the study remained as independent predictors for melanoma-specific survival (p<0.001) including peripheral location of the lesion, tumor thickness, high mitotic rate (≥6/mm2) as well as patient age (≤65 years). Study data also showed that peripheral location had the strongest association with melanoma-specific mortality (OR 11.93; CI 95% 4.77-29.86).
“The reasons underlying differences between peripheral and central CHNM are still unknown. The uneven distribution of CHNM between sexes could be due to the protective role of hair in the scalp, neck and ears, which are generally covered by hair, even in elderly women. Another possible explanation is a greater delay in diagnosis of peripheral CHNM, as lesions located on the scalp or ears are not easily visible to the patient,” the study authors wrote.
Reference
1. Tseng WH, Martinez SR. Tumor location predicts survival in cutaneous head and neck melanoma. J Surg Res. 2011;167(2):192-8.
2. Avilés-Izquierdo JA, RodrÃguez-lomba E, Milla J, Hernández-aragüés I. Peripheral cutaneous head and neck melanoma: Definition, characteristics and impact on survival. J Am Acad Dermatol. 2019.






