- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Differentiating Merkel Cell Carcinoma in Skin of Color
Author(s):
The clinical presentations of Merkel cell carcinoma in patients with skin of color require dermatology providers to be more aware of the nuances in diagnosis and management.
The clinical presentations of Merkel cell carcinoma (MCC) in patients with skin of color require dermatology providers to be more aware of the nuances in diagnosis and management. MCC is an aggressive and rare skin cancer that is more common in patients with lighter skin. However, it can also occur in patients with skin of color. There is an overall increasing incidence of MCC in the general population, with an increased number of reports of MCC occurring in patients with skin of color. MCC typically occurs in white male patients with a history of chronic exposure, those 70 years and older, and those in immunocompromised states.1 Previous studies have shown that Black patients have similar survival outcomes but were more likely to present with advanced MCC disease compared with Hispanic and white patients.1,2
David A Litman/AdobeStock
Clinical Presentations
MCC in patients with skin of color can present differently than in patients with lighter skin tones, including a painless, reddish or purplish nodule or papule on the head or neck. The lesion often is rapidly growing and may ulcerate and bleed. However, MCC may present as a hyperpigmented lesion in patients with darker skin tones that can be misdiagnosed as a benign growth such as a nevus or seborrheic keratosis. Also, Black and Hispanic patients are more likely to have MCC on the skin in areas outside the head and neck areas compared with white patients.1
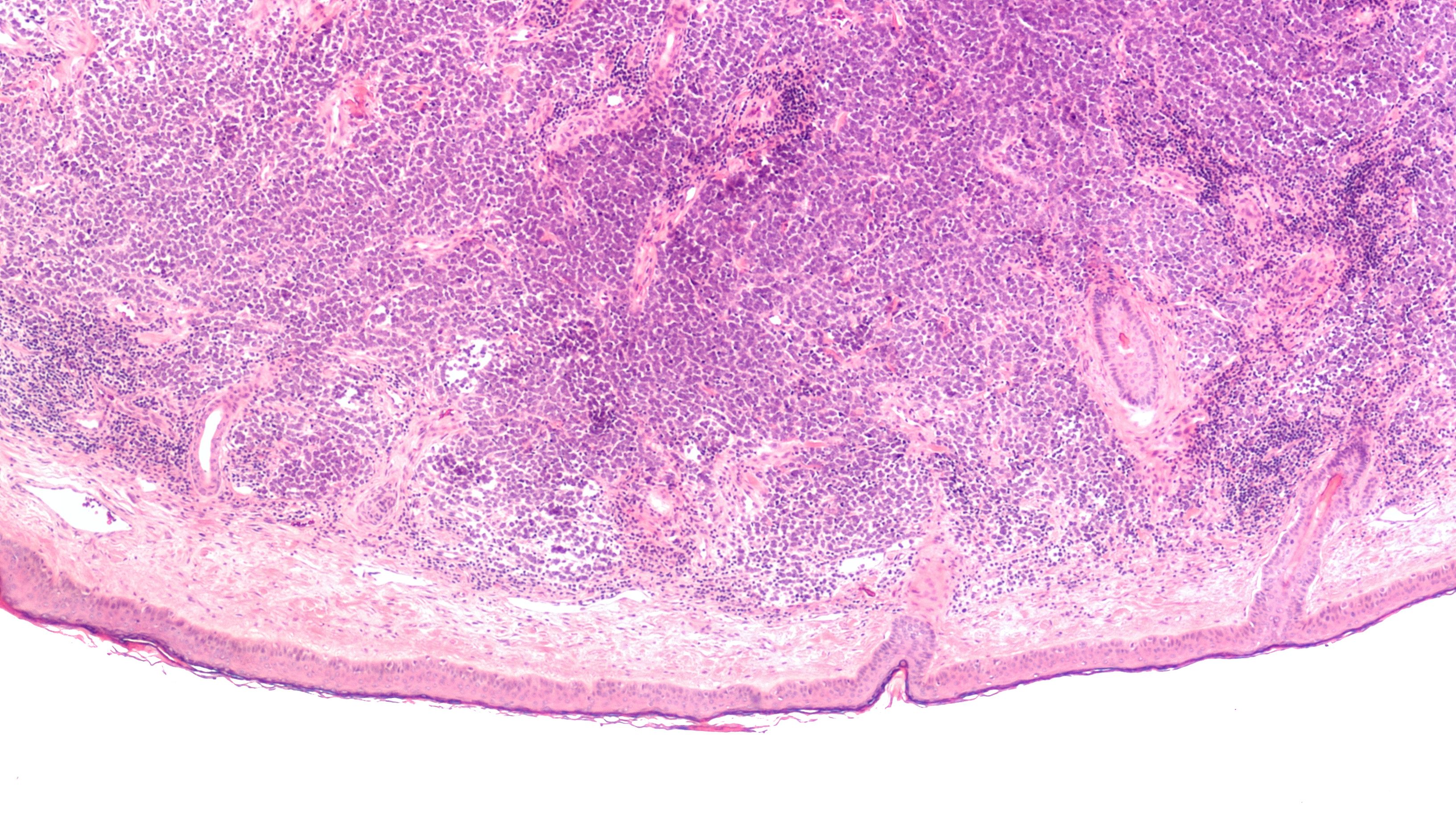
Because it may be more challenging to diagnose MCC in patients with skin color compared with benign pigmented lesions, dermoscopy can be helpful in differentiating MCC. Unlike nevi, MCC tends to have a polymorphous vascular pattern without a blue-gray veil or pigmented structures.3 Further, biopsy is the best way to diagnose MCC. An excisional biopsy or punch biopsy should be performed to obtain a tissue sample for pathology. Immunohistochemistry testing for neuroendocrine markers like cytokeratin 20 and synaptophysin can assist in the diagnosis of MCC.4 It is recommended that patients with advanced MCC at the time of diagnosis receive a sentinel lymphnode biopsy.5
Treatment
The treatment of MCC in patients with skin of color is similar to that of fair-skinned patients. Options include multidisciplinary discussion of the management at tumor board, surgery with wide local excision or Mohs, radiation, and chemotherapy. Mohs surgery for patients with skin of color may be a better option than wide local excision as it may be more difficult to visualize the margins of the tumor.6 Mohs surgery is a highly specialized surgical technique that can improve the assessment of margin control, leading to high cure rates and sparing removal of healthy tissue. If MCC has become metastatic or is recurrent, then radiation therapy is often considered. However, patients with skin of color should be counseled on postradiation therapy dyspigmentation as a cosmetic adverse effect of this treatment.5 Advanced MCC can also be treated with chemotherapy and immunotherapy. Traditional chemotherapy such as bleomycin is associated with a higher risk of hyperpigmentation in patients with skin of color.5
Prevention and Conclusion
Providers should counsel all of their patients on using sun protection to decrease the risk of MCC. Because some sunscreens with physical blockers may leave a white cast on darker skin, some patients may not want to use these formulations. Patients should be informed about tinted sunscreens or formulations that are easily absorbed into the skin to reduce barriers to sunscreen use in this population. Also, skin-of-color patients should be encouraged to practice sun protective behaviors such as wearing protective clothing and seeking shade.2
Overall, MCC is an aggressive and rare skin cancer with increasing incidence in our country. Patients with skin of color are increasingly presenting with more advanced MCC. To provide proactive care, MCC should be considered in the differential diagnosis and biopsied early for these patients with concerning lesions. Diagnosis and management of MCC in this community can be challenging because of the differences in clinical presentations and potential adverse effects from treatment. It is important for dermatology providers to be aware of these differences and to take them into consideration when treating MCC in patients with skin of color.
Nicole Negbenebor, MD, is a Mohs micrographic surgery and cutaneous oncology fellow in the University of Iowa’s Department of Dermatology. After medical school, she trained in the Department of Dermatology at Brown University. She is also a cofounder of the Skin of Color Community Event Series, which increases access to dermatology for underserved populations. She is passionate about Mohs, research, advocacy, skin of color, and cutaneous oncology.
Dr Negbenebor has no relevant disclosures to report.
References
- Mohsin N, Martin MR, Reed DJ, et al. Differences in Merkel cell carcinoma presentation and outcomes among racial and ethnic groups. JAMA Dermatol. 2023;159(5):536-540. doi:10.1001/jamadermatol.2023.0061
- Mosallaei D, Lee EB, Lobl M, Clarey D, Wysong A. Rare cutaneous malignancies in skin of color. Dermatol Surg. 2022;48(6):606-612. doi:10.1097/DSS.0000000000003440
- Jalilian C, Chamberlain AJ, Haskett M, et al. Clinical and dermoscopic characteristics of Merkel cell carcinoma. Br J Dermatology. 2013;169(2):294-297. doi:10.1111/bjd.12376
- Wang TS, Byrne PJ, Jacobs LK. Merkel cell carcinoma: update and review. Semin Cutan Med Surg. 2011;30(1):48-56. doi:10.1016/j.sder.2011.02.001
- Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87(4):733-744. doi:10.1016/j.jaad.2021.12.062
- Carrasquillo OY, Cancel-Artau KJ, Ramos-Rodriguez AJ, Cruzval-O’Reilly E, Merritt BG. Mohs micrographic surgery versus wide local excision in the treatment of Merkel cell carcinoma: a systematic review. Dermatol Surg. 2022;48(2):176-180. doi:10.1097/DSS.0000000000003331