- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Topical Creams Are Important in Atopic Dermatitis Treatment
Author(s):
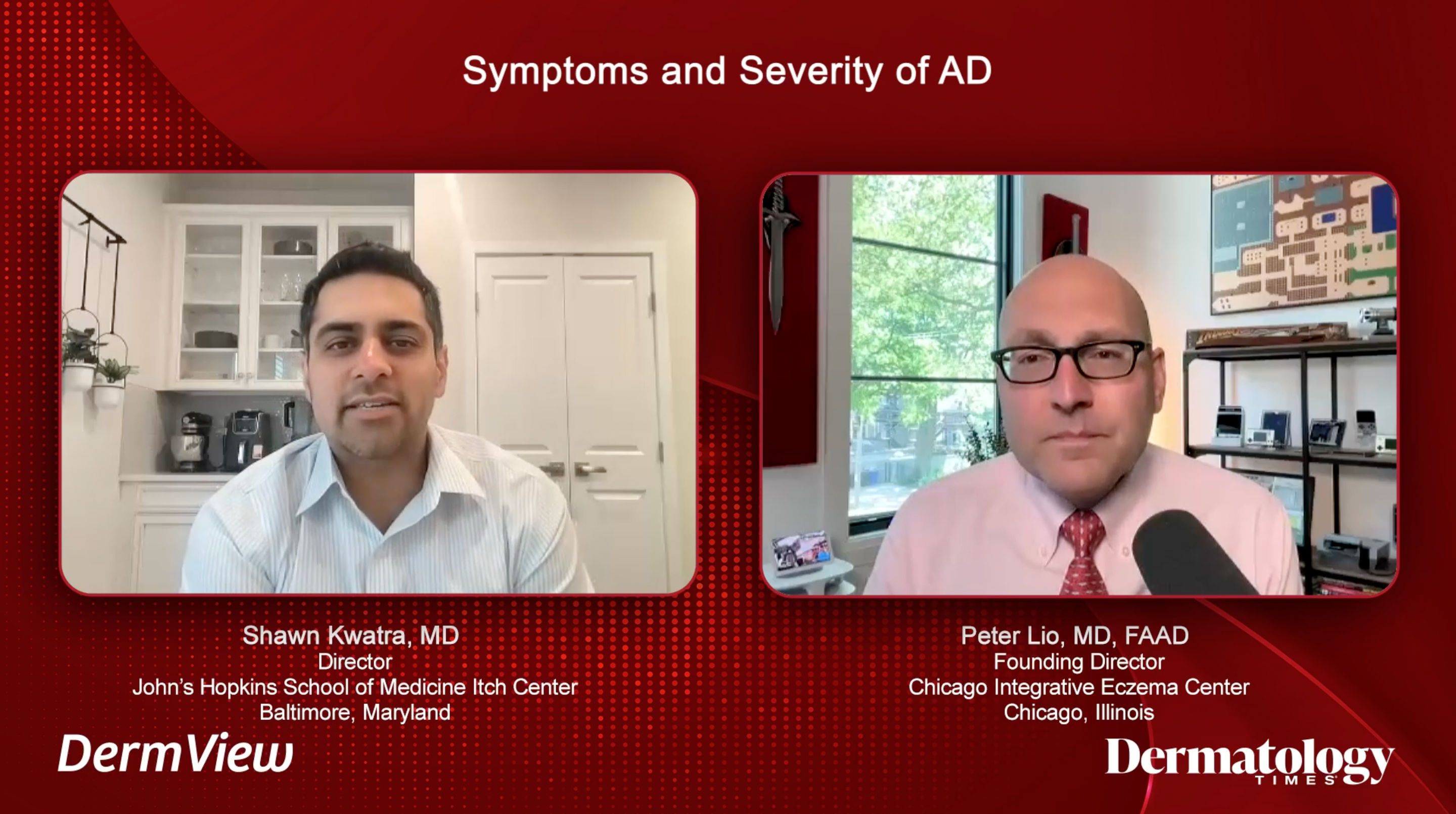
In a Dermatology Times DermView custom video series, Shawn Kwatra, MD, and Peter Lio, MD, discuss the topical treatment landscape of atopic dermatitis.
Topical creams remain one of the most accessible, effective treatment options for patients with atopic dermatitis (AD). In a Dermatology Times DermView custom video series titled “The Power of Topical Creams: Combining BSA and Itch Data for Effective Atopic Dermatitis Management,” Shawn Kwatra, MD, director of the Johns Hopkins Itch Center and associate professor of dermatology at Johns Hopkins University School of Medicine in Baltimore, Maryland, moderated a discussion about the topical treatment landscape. Also participating was Peter Lio, MD, clinical assistant professor of dermatology and pediatrics at Northwestern University Feinberg School of Medicine in Chicago, Illinois.1
Kwatra explained his personal experience with AD and how a flare-up affects his work. “Recently the pollen was just terrible and then my eczema came out of nowhere. I had to leave my lab meeting just so I could scratch and dig in on myself,” he shared. “I hated it because I had to give a talk and I was presenting. I didn’t have my creams or other things [to help with the itch]. It’s the unpredictability that is uniqueto AD.”
Measuring the Severity of an AD Case
Aside from his work at Northwestern University, Lio is also the cofounder and codirector of the Chicago Integrative Eczema Center. He and the center’s team are consistently seeking and advocating treatment options that work for patients, which means enhancing ways to determine the severity of an AD case. “In the last couple of years, I’ve become kind of obsessed with this validated tool for measuring AD control called the Atopic Dermatitis Control Tool [ADCT],” Lio said. The ADCT consists of about 45 seconds of comprehensive questions to help a clinician determine how AD is affecting a patient’s work, school, and sleep routines.2
JAK/STAT Pathway in AD and Inflammation
Dermatologists, now more than ever, have a deeper understanding of how cytokines are not just inflammatory—some can also be direct drivers of itch. Lio said, “We know IL-4 and [IL-]13 seem to be able to stimulate IL-31, the master itch cytokine, binding those nerve endings. And to me, the lesson that still…hasn’t permeated the whole world yet is that in general, this is not a histamine-mediated itch; this chronic itch really is not. And so, we have all these patients, legions of them, on antihistamines, which sometimes for other reasons—if you have seasonal allergy, certainly if you use a first generation, you want to knock somebody out, that soporific effect—that makes sense.”
Lio thinks this is where the JAK/STAT pathway comes in. “We’ve really learned that a lot of these inflammatory cytokines share the next…step in the relay race,” he explained. “So, they bind to their cell surface receptors, IL-4, IL-13, even some of the interferon ones. You know, we have a number of different things, TSLP probably is part of this whole story, as well [as] the alarmins, and then when they bind, inside the cell [are] the JAK and STAT enzymes and they can then trigger nuclear change...on a number of relevant cytokines at a time instead of just targeting them individually.”
Kwatra pointed out a study showing that nonsedating antihistamines are not as effective in itch control and that sedating antihistamines can activate areas of the brain associated with scratch relief.3 He said, “If you’re taking an agent, super sedating—I worry about effects on mental status and even long-term dementia... I think JAK inhibitors in this target pathway are very interesting. In 2017, we know we had this revolutionary moment with dupilumab getting approved, and for us IL-4 and IL-13 really took their place in AD history as being very important mediators. Now what we’re also seeing is that IL-31 is very key for itch induction, but not just IL-31—IL-22 is another important mediator.”
Utilizing Topical Treatment Options
Kwatra and Lio both believe topicals are critical for patients with AD to start providing relief as other regimens are implemented into their day-to-day: gentle cleansers, nonsoap cleanser synthetic detergent, and finding a good moisturizer to apply immediately after showering.
“We’ve seen a bunch of new options.... It wasn’t until 2016 that we got crisaborole, our first new big one.... And then more recently, we finally have a new entry, which is our first topical JAK inhibitor,” Lio said. He credited ruxolitinib with being the most powerful nonsteroidal in his practice given the speed with which it clears AD and provides relief to the patient.
Looking Ahead
Kwatra and Lio expressed excitement about new topical treatments coming down the pipeline. “I think roflumilast topically is currently approved for psoriasis in the US, but coming I think…in development for AD—super exciting. To me, it feels like a refinement or the next step on something like the crisaborole. Again, the phosphodiesterase-4 pathway is gentle, safe, and it seems like there will not be any black box warnings,” Lio shared.
Kwatra expressed optimism for therapies that modulate the microbiome directly or indirectly. “There have been some elegant studies being conducted by [Richard] Gallo [,MD, PhD,] at the University of California San Diego. And we know more about the flares of atopic dermatitis and the thought about giving some of the good bacteria, the good microbiome, microbiome species, even fungi,” Kwatra said.
References
- Kwatra S, Lio P. The power of topical creams: combining BSA and itch data for effective atopic dermatitis management. Dermatology Times. June 26, 2023. Accessed June 26, 2023. https://www.dermatologytimes.com/dermview/the-power-of-topical-creams-combining-bsa-and-itch-data-for-effective-atopic-dermatitis
- Pariser DM, Simpson EL, Gadkari A, et al. Evaluating patient-perceived control of atopic dermatitis: design, validation, and scoring of the Atopic Dermatitis Control Tool (ADCT). Curr Med Res Opin. 2020;36(3):367-376. doi:10.1080/03007995.2019.1699516
- Sánchez-Borges M, Ansotegui I, Jimenez JM, Rojo MI, Serrano C, Yañez A. Comparative efficacy of non-sedating antihistamine updosing in patients with chronic urticaria. World Allergy Organ J. 2014;7(1):33. doi:10.1186/1939-4551-7-33