- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Subclinical mite proliferation linked with erythematotelangiectatic rosacea
Author(s):
Abnormal proliferation of the Demodex mites is frequent among patients with erythematotelangiectatic rosacea (ETR), according to one expert.
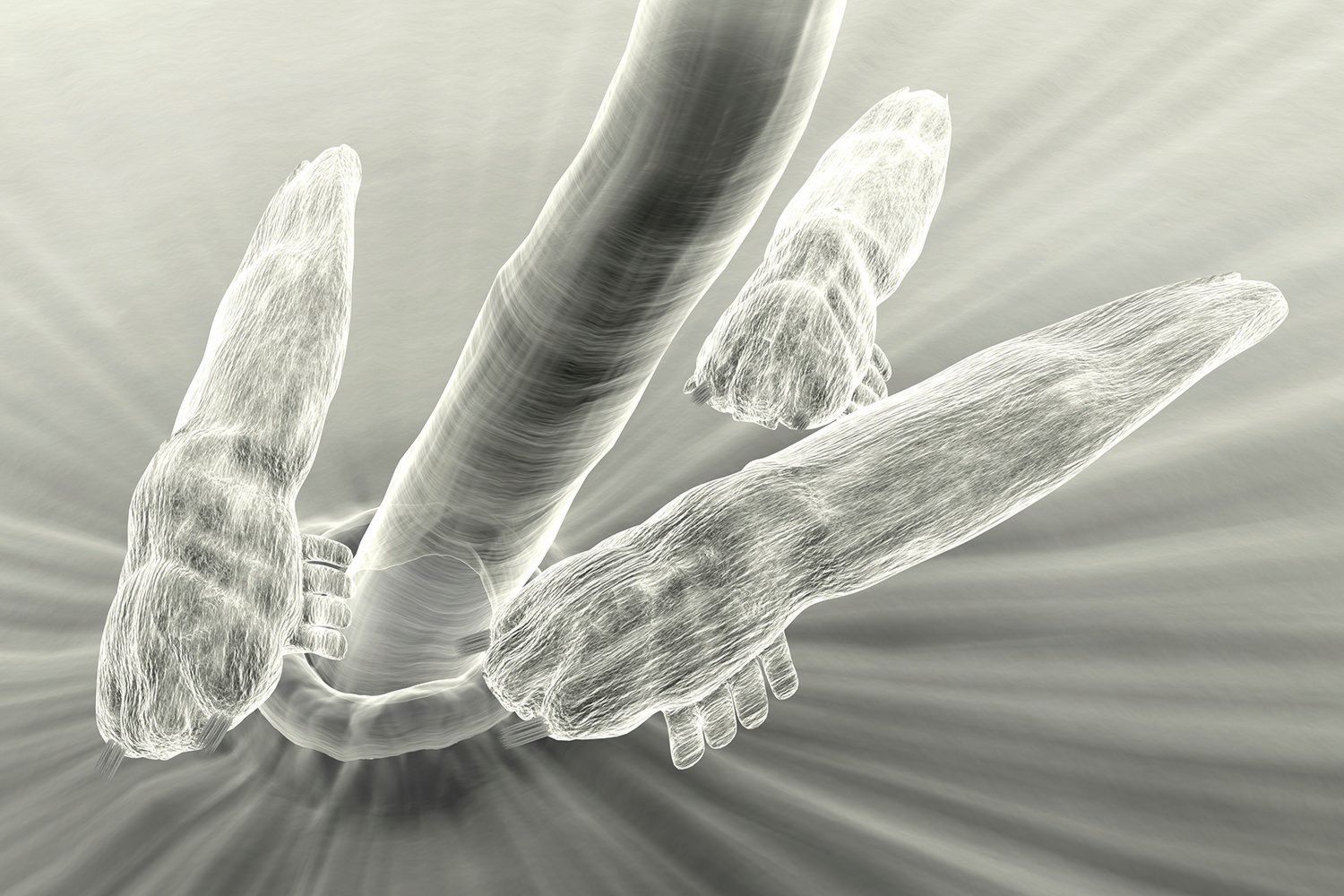
Look for subclinical demodiscosis in patients presenting with erythematotelangiectatic rosacea (ETR), one expert says, because it may represent a therapeutic target for both resolving some signs and symptoms of ETR and perhaps preventing evolution to papulopustular disease.
RELATED: A novel target for rosacea treatment
“Abnormal proliferation of the Demodex mites is frequent among patients with ETR, but it is not always visible to the naked eye,” says Fabienne Forton, M.D., Brussels, Belgium. “Therefore the diagnosis of demodicosis should be considered and Demodex density investigated in any patient consulting for ETR or unexplained subjective complaints that overlap with those of ETR, such as pruritus, burning and hypersensitivity of the facial skin or even of the scalp.”
Although studies investigating the association between infestation with Demodex mites and rosacea have generated conflicting findings, a meta-analysis published in 2017 found that Demodex density was significantly higher in patients with papulopustular rosacea (PPR) as well as those with ETR compared with healthy controls.1 A comparison between the two rosacea cohorts showed that the level of infestation tended to be higher in the subgroup with PPR.1 Dr. Forton and colleague Viviane De Maertelaer, Ph.D., report the same findings in a more recent study.2
If high Demodex density is confirmed, Dr. Forton recommends considering treatment with a topical acaricidal while continuing to monitor Demodex density.
“In our experience, monotherapy with a topical acaricidal to normalize Demodex density may eliminate burning sensation, pruritus, sensitive skin. Although, of course, it does not affect telangiectasias, it may even sometimes improve erythema and flushing and obviate the need for any additional interventions,” says Dr. Forton.
“By preventing further proliferation of the mites, topical acaricidal treatment might also avoid the subsequent immune reaction against these mites and, so, development of PPR.”
RELATED: Oxymetazoline, pulsed dye laser show promise for rosacea
In previous research, Drs. Forton and De Maertelaer showed that Demodex density was significantly higher in patients with PPR or demodicosis compared with healthy controls or patients with other facial dermatoses and similar in the PPR and demodicosis groups.3
To investigate the presence of demodicosis in patients with ETR, they undertook a retrospective study comparing Demodex density measured in two consecutive standardized skin surface biopsies in groups of patients with ETR (n=23), demodicosis (n=590), PPR (n=254), other facial dermatoses (n=180) and healthy controls (n=20).2 They found that the mean Demodex density in the ETR group was significantly greater than that of both the healthy controls and patients with other dermatoses, but significantly less than that of both the PPR and demodicosis groups. Mean Demodex density was approximately eight-fold higher in patients with ETR compared with the healthy controls, and there was an even greater difference between the Demodex density values in the ETR group and the patients with other dermatoses. Mean Demodex densities in the patients with PPR and demodicosis were approximately five- to six-fold greater than in the patients with ETR.
“Notably, 10 (43%) of the 23 ETR patients had Demodex density values that were shown in our previous research to have very high sensitivity and specificity for diagnosing demodicosis and PPR,” Dr. Forton says.
Based on their findings, Dr. Forton and Dr. De Maertelaer suggest that Demodex proliferation may start in ETR or ETR may favor Demodex proliferation. Thereafter, the numerous mites, which eat human cells, disrupt the follicular epithelium and thereby induce the immune reaction observed in PPR. Afterwards, this in ammatory reaction, including vasodilation, exacerbates the ETR, setting up a vicious circle.
“The pathogenic role of Demodex mites in rosacea is further supported by evidence that the mites can trigger a host immune response by activating Toll-like receptor 2, as recently demonstrated by Lacey et al.5 in the first prospective experimental study in this field,” Dr. Forton says.
RELATED: Global panel updates rosacea recommendations
MANAGEMENT IMPLICATIONS
Dr. Forton adds that she has been evaluating patients for demodicosis and rosacea for approximately 20 years and had achieved excellent results treating them with topical benzyl benzoate 20% cream. After Demodex density is normalized and symptoms have disappeared, she continues with maintenance therapy, having patients apply the same cream once a week to prevent reproliferation of the mites and symptom relapse.
Now that topical ivermectin is commercially available; however, Dr. Forton says it has become her treatment of choice, because it is better tolerated than benzyl benzoate, which is a potential irritant and also has anti-inflammatory activity in addition to being acaricidal.
“Ivermectin also has anti-inflammatory activity, but the fact that benzyl benzoate is only acaricidal and still effective for improving the symptoms of PPR further supports the idea that Demodex has a key role in the pathophysiology of rosacea,” she explains.
“I believe that through their experience with the effective use of ivermectin to treat rosacea, the idea of targeting Demodex infestation to treat rosacea is gaining greater acceptance among dermatologists,” Dr. Forton says.
SAMPLING TECHNIQUE
Dr. Forton uses the standardized skin surface biopsy for identifying abnormal Demodex proliferation. This is a non-bloody sampling method in which the super cial part of the skin and the superficial part of the follicular content are sampled, similar to hair removal with glue.
RELATED: Rosacea, breast cancer possibly linked
“This technique is generally well-tolerated by patients, inexpensive and readily available to all dermatologists,” Dr. Forton says.
Over the years, she has refined the sampling methodology to minimize false negatives. In her current approach, she uses ether to clean the skin and the biopsy slide, and then she takes two consecutive standardized biopsies from the same area. High Demodex density is defined by the finding of “>5 mites/cm2 on the first biopsy or >10 mites/cm2 on the second biopsy.”3
The preliminary cleaning of the skin and slide with ether makes it possible to remove the layer of sebum and potential sweat, thus increasing the adhesion of the glue and standardizing the sampling conditions. The second biopsy, which goes deeper, allows increased volume of the analyzed biotope of the mite, generally collecting twice as many mites as the first biopsy, she explains.
ANOTHER PERSPECTIVE
In an editorial commenting on the study by Drs. Forton and De Maertelaer, Jacob P. Thyssen, M.D., professor, Department of Dermatology and Allergy, University of Copenhagen, Hellerup, Denmark, wrote that the research is important because it shows that Demodex density is elevated even in patients with ETR. However, he cautioned against concluding that a topical acaricidal will be effective treatment for ETR.
Dr. Thyssen noted that it remains unclear whether the abnormal mite proliferation is a primary, secondary or even a tertiary event in ETR. Using Staphylococcus aureus overgrowth on the skin of patients with atopic dermatitis as an analogy, he observed that increased density of Demodex in rosacea may arise as a consequence of skin barrier impairment and in ammation rather than being the primary cause. With that in mind, Dr. Thyssen proposed that barrier impairment and in ammation should be the primary targets for therapeutic intervention.
RELATED: Insights on rosacea in skin of color
“There is a strong need for more research to elucidate the pathogenesis of rosacea, and this research should include prospective cohort studies to determine the time course of development of skin in ammation, barrier impairment and Demodex proliferation,” Dr. Thyssen says.
References:
1. Chang YS, Huang YC. Role of Demodex mite infestation in rosacea: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):441-447
2. Forton F, De Maertelaer V. Erythematotelangiectatic rosacea may be associated with a subclinical stage of demodicosis: a case-control study. Br J Dermatol. 2019;181(4):818-825.
3. Forton FM, De Maertelaer V. Two consecutive standardized skin surface biopsies: an improved sampling method to evaluate Demodex density as a diagnostic tool for rosacea and demodicosis. Acta Derm Venereol. 2017;97(2):242-248.
4. Thyssen JP. Are Demodex mites the best target for rosacea treatments? Br J Dermatol. 2019;181(4):652-653.
5. Lacey N, Russell-Hallinan A, Zouboulis CC, et al. Demodex mites modulate sebocyte immune reaction: possible role in the pathogenesis of rosacea. Br J Dermatol. 2018;179:420–430.