- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Should dermatologists embrace AI?
Author(s):
Allan C. Halpern, M.D., discusses what dermatologists need to understand about AI and how it might interact with or disrupt the specialty.
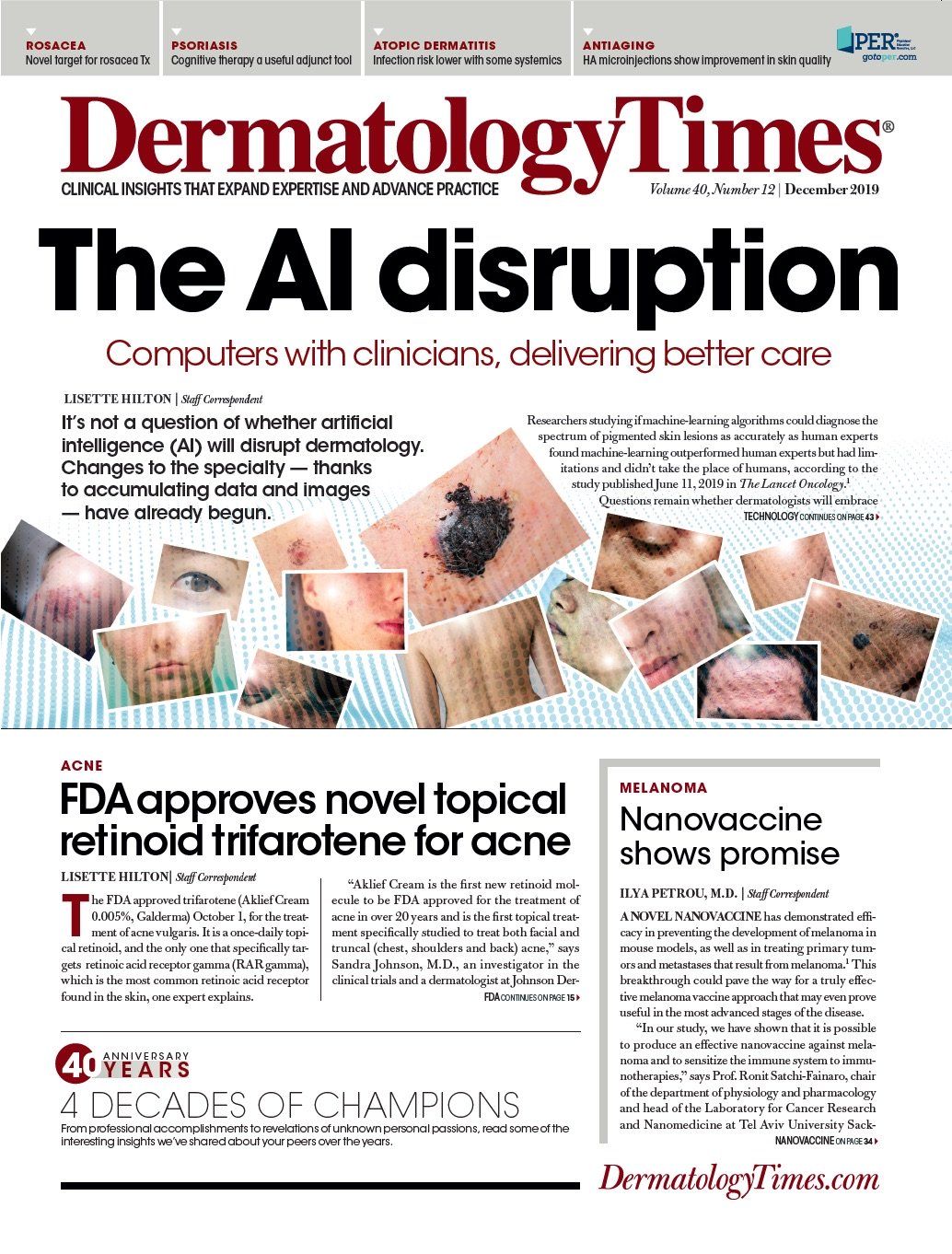
Technology can augment decision making, but cannot replace physicians. (wladimir1804 - stock.adobe.com)

It’s not a question of whether artificial intelligence (AI) will disrupt dermatology. Changes to the specialty - thanks to accumulating data and images - have already begun.
Researchers studying if machine-learning algorithms could diagnose the spectrum of pigmented skin lesions as accurately as human experts found machine-learning outperformed human experts but had limitations and didn’t take the place of humans, according to the study published June 11, 2019 in The Lancet Oncology.1
RELATED: My AI will see you now
Questions remain whether dermatologists will embrace AI and be part of the specialty’s transformation, according to Allan C. Halpern, M.D., chief dermatology service, Memorial Sloan Kettering Cancer Center.
Before answering those questions, dermatologists need to understand AI and how it might interact with or disrupt the specialty, he says.
AI BASICS
“Artificial intelligence is not new,” Dr. Halpern says. “In the 1950s, people used computers to develop what we call expert systems, which frankly worked, but not well. By the 1980s, there were new models for using computers, including machine learning with neural networks, decision trees and more. Since 2012, we’ve been in the third phase: deep learning.”
It’s one thing to describe a set of rules for something like a cat to a computer to recognize (e,g., triangular ears, long tail); it’s another to feed the computer’s memory with thousands of images of all kinds of animals in categories and allow the algorithms to teach themselves. Computers need large image libraries along with accurate associated data to identify animals, or skin lesions, Dr. Halpern explains.
Today’s AI is fueled by the more recently developed “deep learning” algorithms trained on very large data sets. AI “big data” trailblazers like Fei- Fei Li, Ph.D., created ImageNet in 2007. ImageNet is a database of more than 15 million labeled images helping to identify things in some 22,000 categories, he says.
“Computers were all of a sudden amazingly powerful; amazingly fast, and computer memory seemed limitless. They could run newly designed ‘convolutional neural networks,’ which is a fancy way of saying they weren’t constrained to processing in a pre-conceived forward direction. They were allowed to go back to previous premises and rethink as they were learning,” Dr. Halpern says.
RELATED: Artificial Intelligence. Friend or foe of dermatology?
AI made a big splash in dermatology with a cover story published Jan 25, 2017 in Nature2 that indicated AI had the potential to be better than dermatologists, he says.
“There have been a few other examples of papers like this. All show that if you train AI on a reasonable dataset to recognize skin cancer and then you compare how well the computer does to how well dermatologists do, giving them no information except for the picture, the reality is that computers are already as good as dermatologists,” he says.
But, in order to keep training computers, one needs more pictures and more data.
“Computers are just getting pictures with almost no extra data. They don’t know how old the patient is, they don’t know what skin-type the patient is, or if the patient has a previous history of skin cancer, etc.,” Dr. Halpern says.
With more comprehensive data, computers might not only be as good as dermatologists at identifying skin cancer lesions but also at helping to diagnose them.
Art Papier, M.D., CEO of the diagnostic clinical decision support system VisualDx and associate professor in dermatology and Medical Informatics at the University of Rochester, says a growing image library in dermatology and other specialties is helping to train VisualDx and other software algorithms to recognize a spectrum of diseases and disorders.
RELATED: AI: It’s not dermatologist vs. machine
“We’re really talking about machine learning from imagery, in which there’s a flood of innovation in all the visual specialties,” Dr. Papier says. “Radiology, ophthalmology, pathology and dermatology are seeing very rapid advances in the ability to train software to recognize visual patterns.”
The technology not only helps specialists to diagnose conditions they see in the clinic, but it also helps in situations where there are no specialists, such as in rural areas or third-world countries.
“There are some sites in Africa where they only have one dermatologist per million people. Recognition of skin disorders is pushed down to primary care and even healthcare workers. We see a future where our work with VisualDx can assist anybody in recognizing simple rashes, for example. We don’t think that the software is going to pick up some of the nuances that a dermatologist can pick up, so we’re not replacing dermatologists; rather, we’re augmenting the decision making,” he says.
Computer algorithms might also improve differential diagnoses for rare disorders, such as for medication reactions.
“Think about the challenge if a patient comes in, is on multiple medications and has a new rash, one would have to memorize all the adverse events to every medication. What we’ve been doing over the years is tracking all the adverse events to all the drugs so that our dermatologists that use VisualDx can search a medication and instantly see rashes that are causes by that medication,” Dr. Papier says.
WILL COMPUTERS REPLACE ME?
Dermatologists are worried that computers will replace them but that likely won’t be the case, Dr. Halpern says. If AI continues to improve, it will make dermatologists better at what they do, he explains. It would drive the right people to the dermatologist by prescreening away patients whose lesions are benign. Computers could relieve physicians of a lot of the documentation they’re doing today, Dr. Halpern says.
RELATED: Digital tools impact daily dermatology practice
In the future, an acne patient might enter the practice and, with facial recognition, the computer would open his or her chart and determine if the acne improved from the previous visit. The doctor would spend his or her time talking with the patient about optimal care versus feeding the computer information, he says.
AI INITIATIVES IN DERMATOLOGY
Dr. Halpern and colleagues spearheaded the International Skin Imaging Collaboration (ISIC, a collaboration between industry and academia to create the resources to develop image-based algorithms for teaching, research and clinical decision making, he says.
“The reality is most dermatologists don’t take pictures of things. Dermatology is an imaging poor specialty, even though we’re a very visual specialty,” Dr. Halpern says. “Part of what needs to happen if we’re going to take advantage of AI is we need to start doing imaging very routinely in our practices, and we need to start setting the groundwork for AI to become good enough to become helpful to us.”
One of the problems is there are no standards for imaging in dermatology. Unlike in specialties like radiology where x-ray images are similar regardless of who takes them, no two dermatologists take pictures in the same way. As a result, ISIC is developing standards so dermatologists can contribute and share more images with one another and with computers, according to Dr. Halpern.
“The other thing that we’re trying to do is develop a playground of images the same way that Fei-Fei Li did at ImageNet. We’re trying to develop an archive of images for dermatology that everybody can use,” he says.
ISIC’s image archive has tens of thousands of images that are in the public domain and are available for teaching, learning and research, he says. In the last three years, ISIC has hosted three annual computer science challenges at computer science meetings around the world.
“From year to year, the number of images increased, the number of diagnoses represented by the pictures increased, and the number of experts that we compared the computer results to increased,” he says. “…from 2016 to 2017 and 2018 the computers got better and better at diagnosing images and doing it with more diagnoses. In 2018 we compared the three best computer algorithms with over five hundred clinicians from around the world doing 30 images each to see who got more right - the computers or the doctors. Across the entire group, the computer algorithm outperformed the humans on average by two more correct image diagnoses per batch and in some subset analyses the computer outperformed the humans by an average of seven images per batch.”
ISIC collaborations also have resulted in more than 200 scientific papers.
Building the image database is important to dermatology because trying to train the computers without enough images might result in biased algorithms, according to Dr. Halpern.
It’s also important that dermatologists get on board with AI, he says. That way, dermatologists drive AI’s progress.
“If we do this right, it has potential at every level. So, patients can end up with apps that help them find information that might help them avoid unnecessary visits to the dermatologist or to any clinician. AI might help advanced practice providers deliver better care in dermatology practices and other types of clinics. Even those of us who are ‘expert physicians’ will benefit from this,” he says. AI could help make dermatologists practice more efficiently and to their full potential, Dr. Halpern says.
“We can be there making the really tough clinical decisions and actually engaging with our patients over how we get them better and how we take care of them,” Dr. Halpern says. “The whole idea is it’s not about computers against clinicians, it’s really computers with clinicians delivering better care.”
Disclosures:
Dr. Halpern is a consultant with Canfield Scientific, Lucid and SciBase.
References:
1. Tschandl P, Codella N, Akay BN, et al. Comparison of the accuracy of human readers versus machine-learning algorithms for pigmented skin lesion classification: an open, web-based, international, diagnostic study. Lancet Oncol.2019;20(7):938-947.
2. Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-118.