- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Racial disparities in psoriasis treatment
Author(s):
A recent study explored why black individuals with psoriasis are disproportionately under treated. Authors compared differences in the perceptions and understanding of psoriasis therapies in both black and Caucasian patients. Here’s what they found.
Study suggests that there is more unfamiliarity with biologic therapy in black individuals compared to caucasian patients. (©M0M0TaR0/Shutterstock.com)

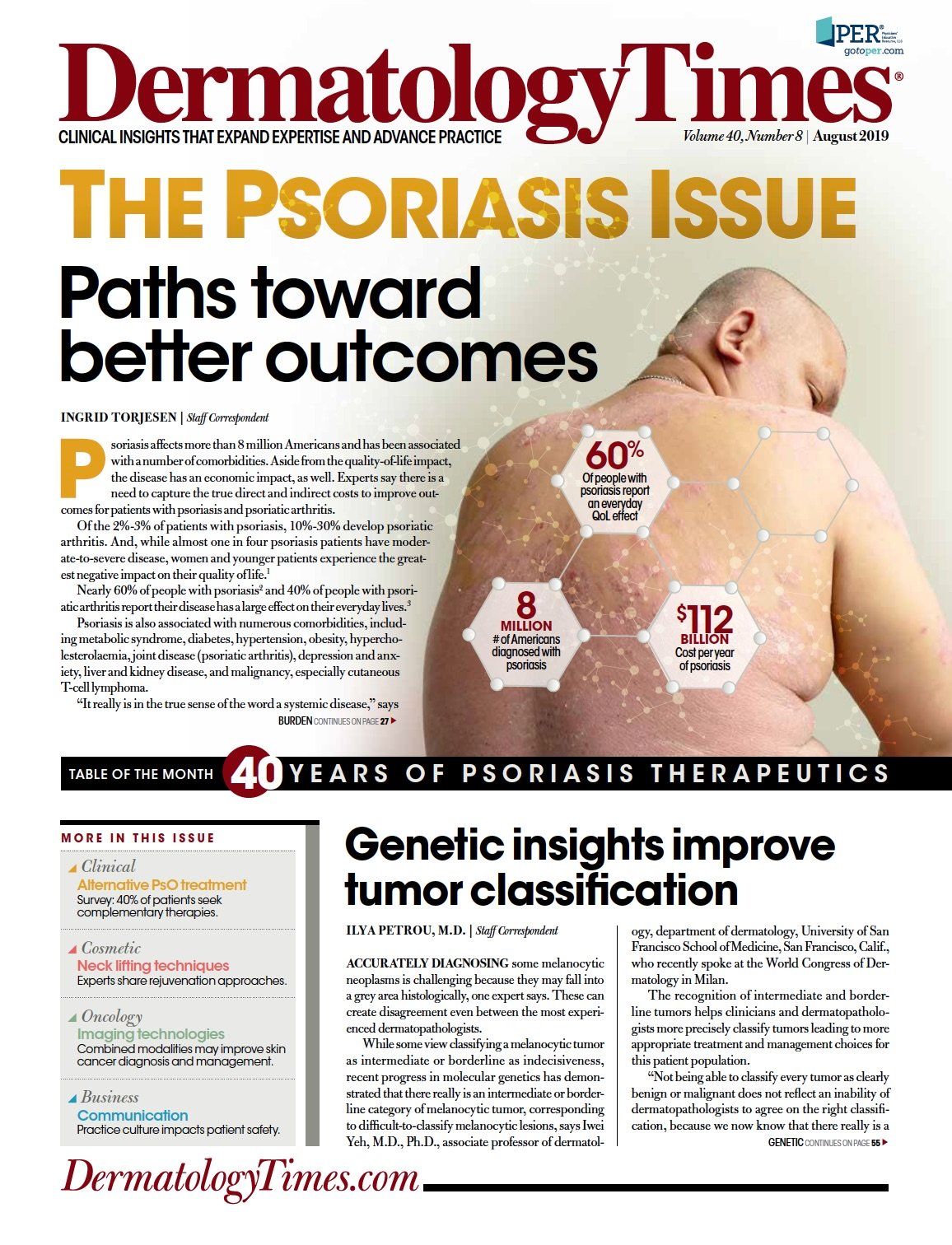
Psoriasis is a common skin disorder that is associated with cardiometabolic disease that negatively impacts psychosocial well being. According the National Psoriasis Foundation, 7.5 million Americans suffered from psoriasis in 2018. There are a growing number of efficacious medications to treat this skin disease, but still many patients remain under treated.
Dr. Junko Takeshita and colleagues in the Department of Dermatology, Perelman School of Medicine, University of Pennsylvania, Philadelphia hypothesized that under treatment may disproportionately affect minorities. These researchers designed a qualitative study using “free-listing” to understand and compare perceptions of biologics and other common or newer psoriasis therapies among white and black individuals with moderate to severe plaque psoriasis who had not received biologic treatment. The results were published in February in the Journal of Investigative Dermatology.
Free-listing is a well established method, in which the patient is asked to list all words they think of in connection with a word or phrase. This method allowed the researchers to identify psoriasis patients attitudes towards biologic therapies.
68 patients were included in the study. Patients included all shared similar psoriasis histories. Half the patients were caucasian while the other half were black. Free-listing results were obtained for the following words: infliximab, apremilast, methotrexate, phototherapy and self-injecting biologics.
Lack of familiarity with treatment was the most or second most salient item for all other psoriasis therapies. The study showed, however, that there were differences in perceptions and understanding of psoriasis therapies between the two racial groups.
The greatest difference was found in self-injectables where many black biologic naive patients used ‘unfamiliar’ as their salient word. Surprisingly, this difference was not impacted by income or education level.
Based on the studies results the authors hypothesize that there is more unfamiliarity with biologic therapy in black individuals compared to caucasian patients. This is a potential modifiable cause of racial disparity in psoriasis therapy.