- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
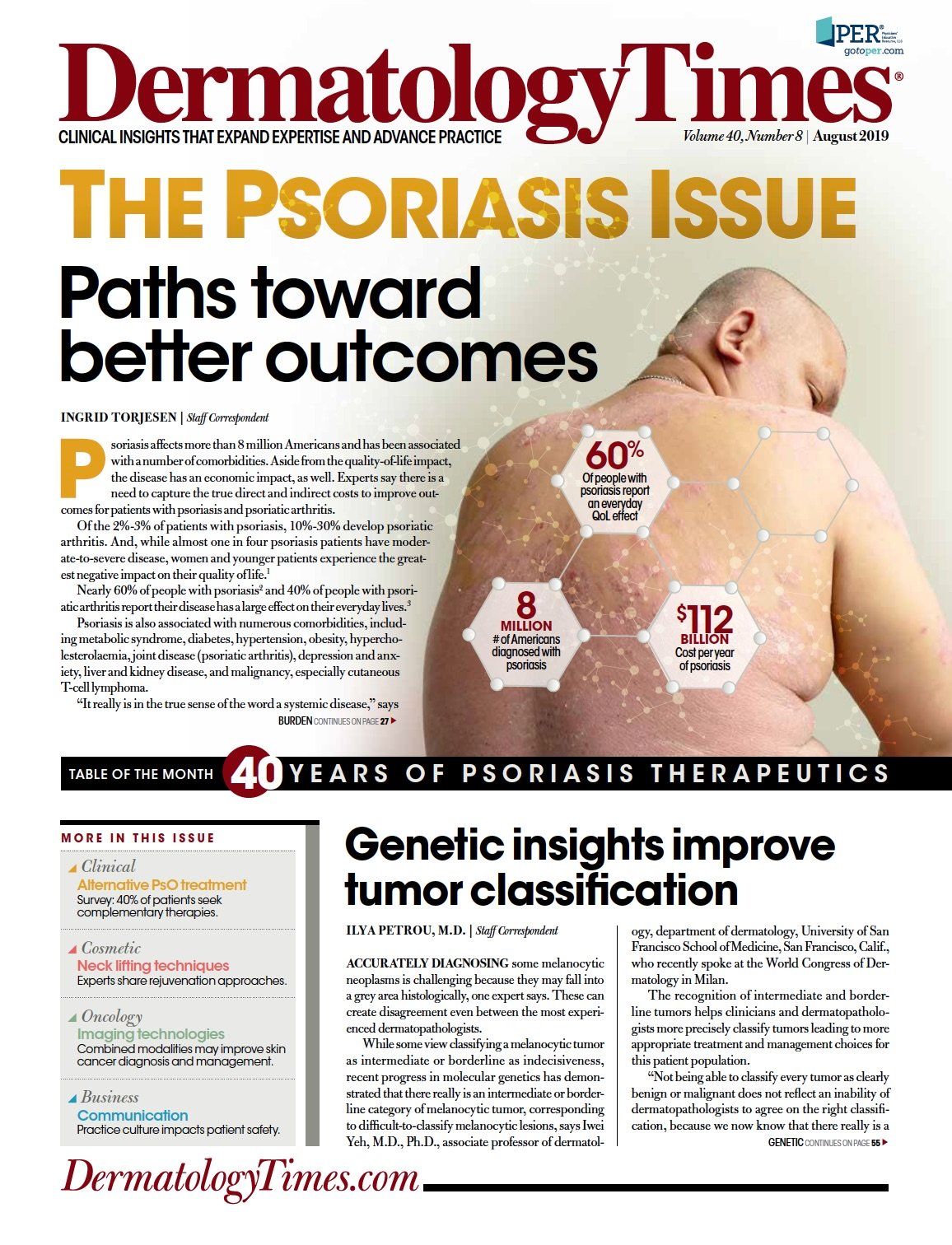
Publication
Article
Dermatology Times
Lifting the psoriasis burden
Author(s):
Psoriasis patients face a long list of comorbidities, increased medical costs and increased mortality. Experts agree that the burden of psoriasis is heavy - what can dermatologists do to offer relief?
“A substantial proportion of patients with psoriasis have comorbid conditions that should be considered when formulating a treatment and management plan,” says Steven Feldman, M.D. (Nikkikii - stock.adobe.com)

Dr. Van Voorhees

Dr. Armstrong
Dr. Feldman
Psoriasis affects more than 8 million Americans and has been associated with a number of comorbidities. Aside from the quality-of-life impact, the disease has an economic impact, as well. Experts say there is a need to capture the true direct and indirect costs to improve outcomes for patients with psoriasis and psoriatic arthritis.
Of the 2%-3% of patients with psoriasis, 10%-30% develop psoriatic arthritis. And, while almost one in four psoriasis patients have moderate-to-severe disease, women and younger patients experience the greatest negative impact on their quality of life.1
Nearly 60% of people with psoriasis2 and 40% of people with psoriatic arthritis report their disease has a large effect on their everyday lives.3
Psoriasis is also associated with numerous comorbidities, including metabolic syndrome, diabetes, hypertension, obesity, hypercholesterolaemia, joint disease (psoriatic arthritis), depression and anxiety, liver and kidney disease, and malignancy, especially cutaneous T-cell lymphoma.
“It really is in the true sense of the word a systemic disease,” says Abby Van Voorhees, M.D., professor and chair of dermatology at Eastern Virginia Medical School, Norfolk, Va.
Patients with psoriasis also have an increased risk of early death,4 particularly from the consequences of cardiovascular disease, such as myocardial infarction.5 Cardiovascular disease appears to occur earlier in patients with psoriasis - and the increased risk is similar to that related to diabetes, she adds.
A real-world study looking at U.S. patients with psoriasis found the most prevalent comorbidities to be hyperlipidemia (48.6%), hypertension (44.7%), depression (18.7%), type 2 diabetes mellitus (18.3%), and obesity (15.0%).6
“A substantial proportion of patients with psoriasis have comorbid conditions that should be considered when formulating a treatment and management plan,” says Steven Feldman, M.D., of the department of dermatology, Wake Forest University School of Medicine, Winston-Salem, N.C., who was a researcher on this study.
“These conditions can complicate treatment of patients with psoriasis. The choice of treatment may have intended or unintended effects on some of the common comorbidities,” he adds.
The presence or absence of certain comorbidities can drive some physicians toward or away from various treatments, according to Dr. Van Voorhees.
For example, if a patient with psoriasis also has an inflammatory bowel disease, such as Crohn’s, she says she will try. to avoid using an IL 17 agent because that could potentially make the Crohn’s disease worse. However, if the patient with psoriasis also has psoriatic arthritis, she will actively choose an IL 17 or a TNF inhibitor, because they are known to be highly effective in both conditions. There also is early evidence to suggest that if patients with psoriatic arthritis are treated with TNF inhibitors it reduces the risk of overall mortality and cardiovascular comorbidity, she adds.
ECONOMIC IMPACT
Aside from the increased morbidity and mortality, psoriasis has a substantial impact on patients’ pockets. Those with severe psoriasis have a much lower earning potential than those in the general population, as they often have to take time out of the workplace to attend doctors’ appointments and treatment and/or take sick leave because their skin is painful, Dr. Van Voorhees says.
“There is no question that this impacts people’s livelihoods quite substantially, and probably part of that is active choices on the part of the patient,” she says.
Psoriasis mostly commonly starts in the late teens or early 20s - a time when people are making their career choices, she says. You can imagine a patient weighing job opportunities that enable them to get to treatments and appointments, whereas someone who does not have psoriasis wouldn’t have the same considerations.
Psoriasis also has a substantial economic impact on the health systems responsible for their care and the wider economy, although the full extent of the economic is difficult to quantify.
One of the most comprehensive analyses to date is a systematic review that attempted to quantify the costs of psoriasis in the United States in 2013. The review evaluated 22 studies and put the cost of psoriasis at $112 billion per year comprising direct medical costs of $51.7 billion to $63.2 billion, indirect costs of loss of productivity from absenteeism and presenteeism at work of $23.9 billion to $35.4 billion and the medical costs associated with treating comorbidities of $36.4 billion. The economic impact of psoriasis was found to be greatest for patients with
more severe psoriasis and comorbidities, in particular psoriatic arthritis, depression or anxiety.
April Armstrong, M.D., of the department of dermatology, University of Colorado, Denver, and a reviewer, says the figures were likely an underestimate of the total cost burden.
“A pressing need exists to conduct a comprehensive study from a societal perspective that captures the direct, indirect, intangible, and comorbidity costs associated with psoriasis,” she says.
It is also important for studies examining the costs of systemic therapies for moderate-to-severe psoriasis to take account of their cost-effectiveness, not just their direct costs, she adds.
“Long-term cost-effectiveness models for systemic and biologic drugs are needed to provide valuable algorithms for treatment selection,” Dr. Van Voorhees says.
Surveys by the National Psoriasis Foundation and formal studies have shown that a large number of patients with psoriasis in the United States are frequently dissatisfied with the medical treatment they receive for their condition.
“It is not surprising,” says Dr. Van Voorhees, chair of the National Psoriasis Foundation medical board, “because even amongst those with very severe psoriasis, most of them are not on any kind of systemic agent at all. Most are using a topical steroid and often not even that. You really have a population who doesn’t feel that their needs for their skin or being met.”
This undertreatment is a combination of patients not being prescribed the most effective drugs because they are not covered by insurance, doctors deciding to offer only a topical because of the difficulties in getting approval for a systemic agent, and patients being concerned about taking systemic agents because of potential side effects, she explains.
“The onus is on us as their caregivers to make sure that we get their skin clear or almost clear and that often requires a systemic agent,” she says. These drugs are generally well tolerated and can be “life changing in terms of the profoundness of the effect they can have on people when their skin clears.”
Phototherapy continues to represent an important mainstay of treatment for patients who do not want to take systemic agents and have the time to attend sessions, Dr. Van Voorhees adds.
“Phototherapy is really like a systemic therapy in my mind, because it really is causing - through the skin - a reduction in the inflammation of the skin. I almost think of it as like a transdermal anti-inflammatory treatment.” Â
References:
1. Gelfand JM, Feldman SR, Stern RS, Thomas J, Rolstad T, Margolis DJ. Determinants of quality of life in patients with psoriasis: a study from the U.S. population. J Am Acad Dermatol. 2004 Nov;51(5):704-8.
2. Stern RS, Nijsten T, Feldman SR, Margolis DJ, Rolstad T. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc. 2004 Mar;9(2):136-9.
3. Gelfand JM, Gladman DD, Mease PJ, Smith N, Margolis DJ, Nijsten T, Stern RS, Feldman SR, Rolstad T. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005 Oct;53(4):573.
4. Springate DA, Parisi R, Kontopantelis E, Reeves D, Griffiths CE, Ashcroft DM. Incidence, prevalence and mortality of patients with psoriasis: a U.K. population-based cohort study. Br J Dermatol. 2017 Mar;176(3):650-8.
5. Wu JJ1, Choi YM, Bebchuk JD. Risk of myocardial infarction in psoriasis patients: a retrospective cohort study. J Dermatolog Treat. 2015;26(3):230-4.
6. Shah K, Mellars L, Changolkar A, Feldman SR. Real-world burden of comorbidities in US patients with psoriasis. J Am Acad Dermatol. 2017;77:287-92.
7. Brezinski EA, Dhillon JS, Armstrong AW. Economic Burden of Psoriasis in the United States: A Systematic Review. JAMA Dermatol. 2015;151(6):651-8.
8. Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149(10):1180-5.
9. Korman NJ, Zhao Y, Pike J, Roberts J, Sullivan E. Patient satisfaction with current psoriasis treatment: a real-world study in the USA. Dermatol Online J. 2016;22(2).