- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
News
Article
Dermatology Times
Guidelines for Surgical Treatment of Early-Stage Vulvar Squamous Cell Carcinomas
Author(s):
Collaboration between dermatologists and gynecologists can improve patient quality of life and outcomes in vSCC treatment.
A recent literature review1 published in the International Journal of Women’s Dermatology examined gynecology guidelines for the management of vulvar squamous cell carcinomas (vSCC) to better inform dermatologic surgeons of when and why to escalate patient care. From their review, Rao et al recommended that dermatologists should be aware of the guidelines used by other specialists treating vSCC “due to the morbidity associated with the disease in this region."
“Dermatologic surgeons often play an important role in the treatment of these malignancies and therefore need to understand the difference in the gynecology-oncology guidelines compared to more commonly treated tumors in other locations. In particular, lymph node biopsy or radical vulvectomy, is recommended for many of these SCCs. Dermatologic surgeons should be aware of these guidelines to inform their clinical plans,” said study author Elizabeth Rao, a fourth-year medical student in the department of dermatology at Case Western Reserve University School of Medicine in Cleveland, Ohio.
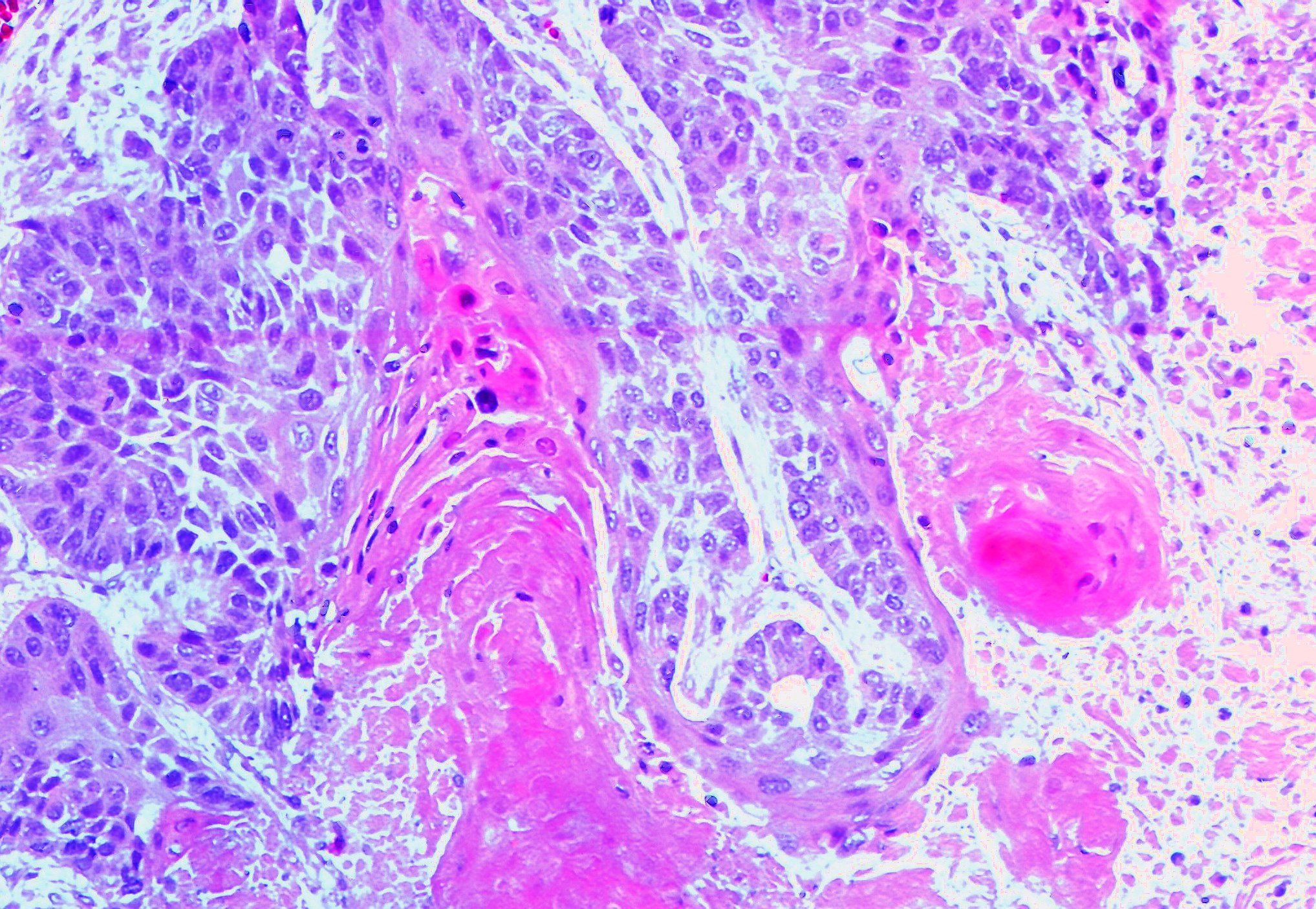
Regarding what is currently known about vSCC and its effect on women and their families, Rao et al noted that vSCCs are the most common vulvar carcinomas, representing almost 90% of all vulvar carcinomas, and have an increased chance for significant morbidity and negative impact on quality of life due to the proximity of the tumors to the clitoris, urethra, vagina, anus, and inguinofemoral lymph nodes.
Currently, Mohs micrographic surgery (MMS) and advantageous intraoperative margin assessments are known treatments for early-stage vSCC. When treating early-stage tumors, gynecologists may use wide local excision, radical vulvectomy, lymph node dissection, and adjuvant chemoradiation for specific cases. For dermatologists, recognizing and understanding gynecologic-oncology recommendations helps to understand when it is the right time to escalate treatment to provide patients with the best care.
To collect up-to-date treatment guidelines to better inform dermatologic surgeons, Rao et al performed a literature review by searching for the terms “vulvar,” “squamous cell carcinoma,” “treatment,” and “guidelines” together in PubMed and Google Scholar using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Of the first 341 results, 18 articles remained after screening for updated versions and English language. Of the 18 postscreened results, 13 articles related to the surgical treatment of early-stage vSCCs were included in the literature review.
According to Rao et al, vSCCs "are staged by the [International Federation of Gynecology and Obstetrics] (FIGO) 2021 classification and the American Joint Committee on Cancer staging. Early-stage tumors are FIGO stage IA-IB or American Joint Committee on Cancer stage TI-TII, and under 4 cm in size, without suspicion of nodal involvement. Tumors larger than 4 cm in diameter or involving local structures such as the urethra are considered locally advanced and may follow a different treatment paradigm. FIGO stage IA tumors are under 2 cm in diameter, with less than 1 mm stromal involvement; stage IB are those greater than 2 cm or with greater than 1 mm depth.”
The study authors noted that many guidelines recommend FIGO stage IA, unifocal tumors undergo local excision with minimum 8-mm margins on fixed tissue, while other societies recommend conservative 1- to 2-cm margins.
Guidelines from the German Society for Gynecology and Obstetrics and the German Cancer Society state that margins of 3 mm measured histologically may be acceptable. Adjuvant radiation therapy should be considered for diffuse disease, deep invasion (>1 mm), or close margins (<8 mm). For residual tumors, guidelines recommend reexcision or radiation therapy for unresectable tumors. For tumors invading deeper than 1 mm and extending greater than 2 cm, guidelines recommend escalation to radical vulvectomy or radical local excision, according to Rao et al’s review.
Lastly, the collected guidelines determined that lymph node dissection via sentinel lymph node biopsy or inguinofemoral node dissection is recommended for FIGO stage IB and higher or depth of invasion greater than 1 mm. Lateral tumors (>1 cm from midline) should undergo ipsilateral unilateral lymph node biopsy and midline lesions should undergo bilateral lymph node biopsy.
“I hope that dermatologists recognize that they can and should help in the treatment of these malignancies. However, given the current guidelines, this may be a partnership with a gynecological oncologist. The current recommendations are very different than the treatment of similar tumors in other locations. We need further research into margin size and metastatic risk in vulvar SCC to better inform how we best utilize Mohs micrographic surgery to perform accurate, tissue sparing surgery in this sensitive area, especially as treatments continue to advance,” said Rao.
From their literature review, Rao et al encouraged dermatologists to be aware of the guidelines used by gynecologists/oncologists for the treatment of vSCC to better improve the quality of life of patients and to decrease the risk of morbidity. The authors also mentioned that there is limited data on the recurrence rates of vSCC after MMS and additional research may contribute to the evolving treatment guidelines.
“Guideline-based vSCC treatment includes faster escalation to radical vulvectomy and lymph node dissection than other high-risk sites treated by MMS such as facial mask areas. More narrow margins of [greater than]3 mm on fixed tissue may be acceptable. Further research on margin size in vSCC may inform treatment focused on tissue conservation or intraoperative margin assessment, hallmarks of MMS,” the authors wrote.
“Women’s health care, particularly vulvovaginal disorders, is an area that could always use more research and more attention. Disorders of the vulvovaginal area can have large impacts on quality of life. I’m glad there is increasing attention paid to women’s health in dermatology because it is so important to our patients to continue building our repertoire of treatments through research, collaboration, and innovation. Patients may see dermatologists or gynecologists first for these issues too, and so teamwork between specialties is crucial. I was lucky to have mentors in both gynecology-oncology and dermatology on this project,” concluded Rao.
Reference
- Rao EM, Wilkowski CM, DeSouza L, McNally A, Lucas J. Surgical treatment of early-stage vulvar squamous cell carcinomas: a systematic review of guidelines for dermatologic surgeons. Int J Womens Dermatol. 2023;9(3):e104. doi:10.1097/JW9.0000000000000104