- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Mechanisms driving melanoma immunotherapy
Author(s):
Dermatologists should work to gain a better understanding of immunologic pathways as well as the mechanisms of new and evolving immunotherapies, as these are key for understanding many current and emerging melanoma treatments, one expert says.
“I consider dermatologists as the primary care physician for melanoma patients and, as such, it is good for us to be well versed in this specific field," says Delphine J. Lee, M.D. (lavizzara - stock.adobe.com)
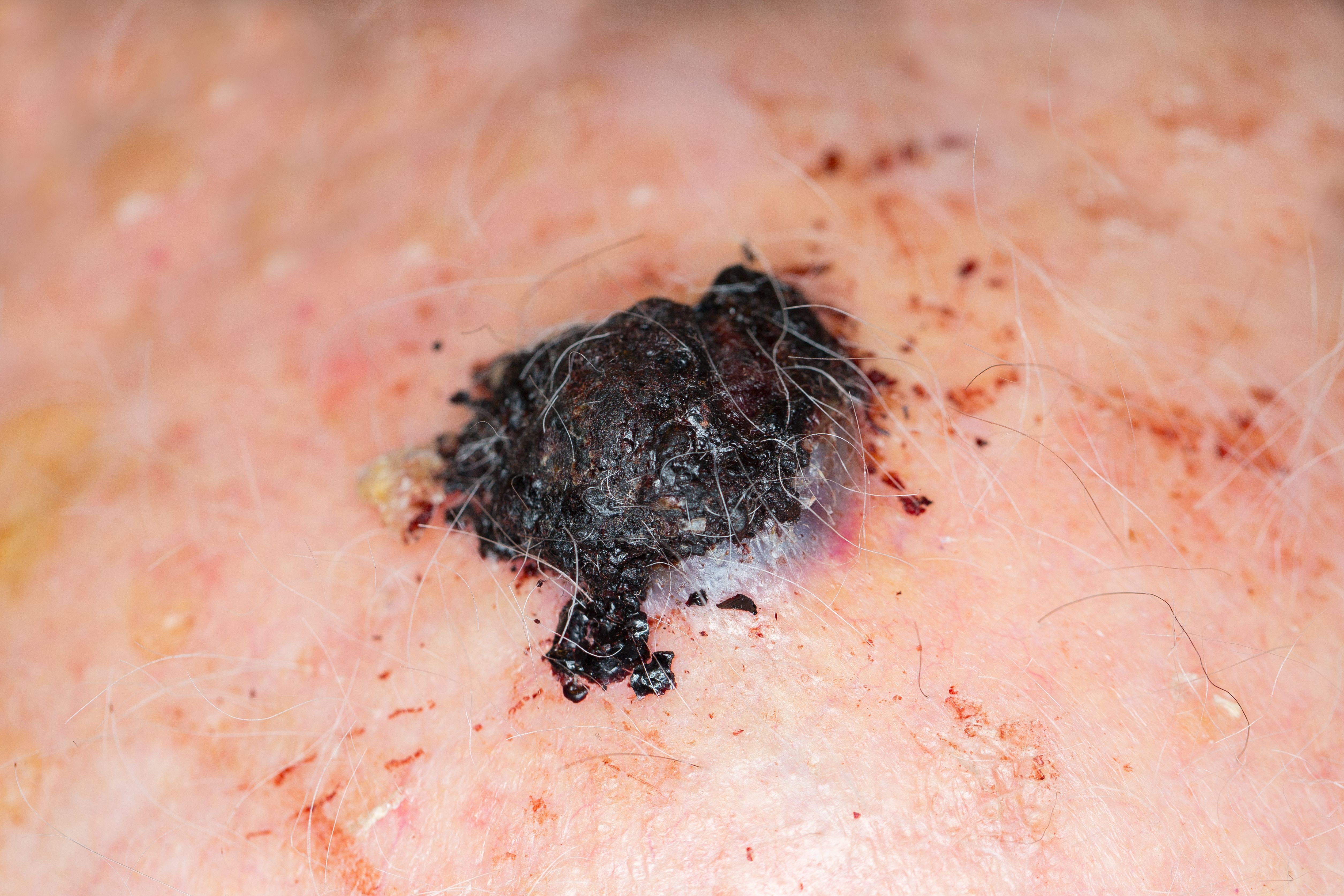
New immunotherapy medications have shown a durable clinical benefit in cancer patients, including those with malignant melanoma. It is important for clinicians to understand the intricacies of the immune mechanisms driving these evolving immunotherapies in order to provide guidance when patients seek advice on best treatment and management strategies, one expert says.
“Melanoma is one type of cancer that is most relevant when it comes to tumor immunology since it is one of the most immunogenic tumors. As such, it should be one of the central goals of dermatologists to gain a better understanding of immunologic pathways as well as the mechanisms of new and evolving immunotherapies, as these are key for understanding many current and emerging treatments,” says Delphine J. Lee, M.D., chief of dermatology and residency program director at Harbor UCLA Medical Center, Los Angeles.
There are several melanoma immunotherapies that have been approved by the U.S. Food and Drug Administration (FDA), including immune checkpoint inhibitors, adoptive cell transfer, as well as vaccines like Bacillus Calmette–Guérin and cytokines that can be used to enhance the host’s immune response to fight the tumor.
Antibodies against the immune checkpoint regulators, such as ipilimumab (Yervoy, Bristol-Myers Squibb), nivolumab (Opdivo, Bristol-Myers Squibb) and pembrolizumab (Keytruda, Merck) have all shown benefit in survival.
According to Dr. Lee, adjuvant immunotherapy is an exciting area of treatment. Just a few years ago those patients who had lymph node involvement (stage 3 disease) were either observed, received interferon alfa or radiotherapy, or could hope to enter a clinical trial after their definitive surgery.
Today, melanoma patients have an increasing variety of immunotherapy medications that can be wisely chosen once they are considered NED (No Evidence of Disease), which will hopefully prolong survival.
“In the past, we just didn’t understand how to manipulate the immune system in the right way. Back when we were making the vaccines in the 1980s, we did not know about immune checkpoint molecules. Now that we understand so much more about the immune system and how it is regulated, we are able to offer our patients advanced immunotherapies that help them improve their survival. It’s just so amazing and great to witness the positive changes that have happened in melanoma therapy in the last few years,” Dr. Lee says.
FUTURE OPTIONS
Future treatment approaches may consist of personalizing therapy one step further. For example, a patient’s novel tumor neoantigens would be identified and, after determining which ones are most highly expressed, vaccines would be developed against those tumor antigens so the patient’s immune system could recognize them.
“I consider dermatologists as the primary care physician for melanoma patients and, as such, it is good for us to be well versed in this specific field. As dermatologists, sometimes we get so busy and have so many patients, but we should not fall in the trap of giving up our more complicated patients after they are referred to other specialists. We will still see them in follow-up for monitoring and screening for new primary lesions or recurrences,” Dr. Lee says. Â
Disclosures:
Dr. Lee reports the following disclosure: Biogen – SH(NC).