- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Leg psoriasis improves with topical lotion
Author(s):
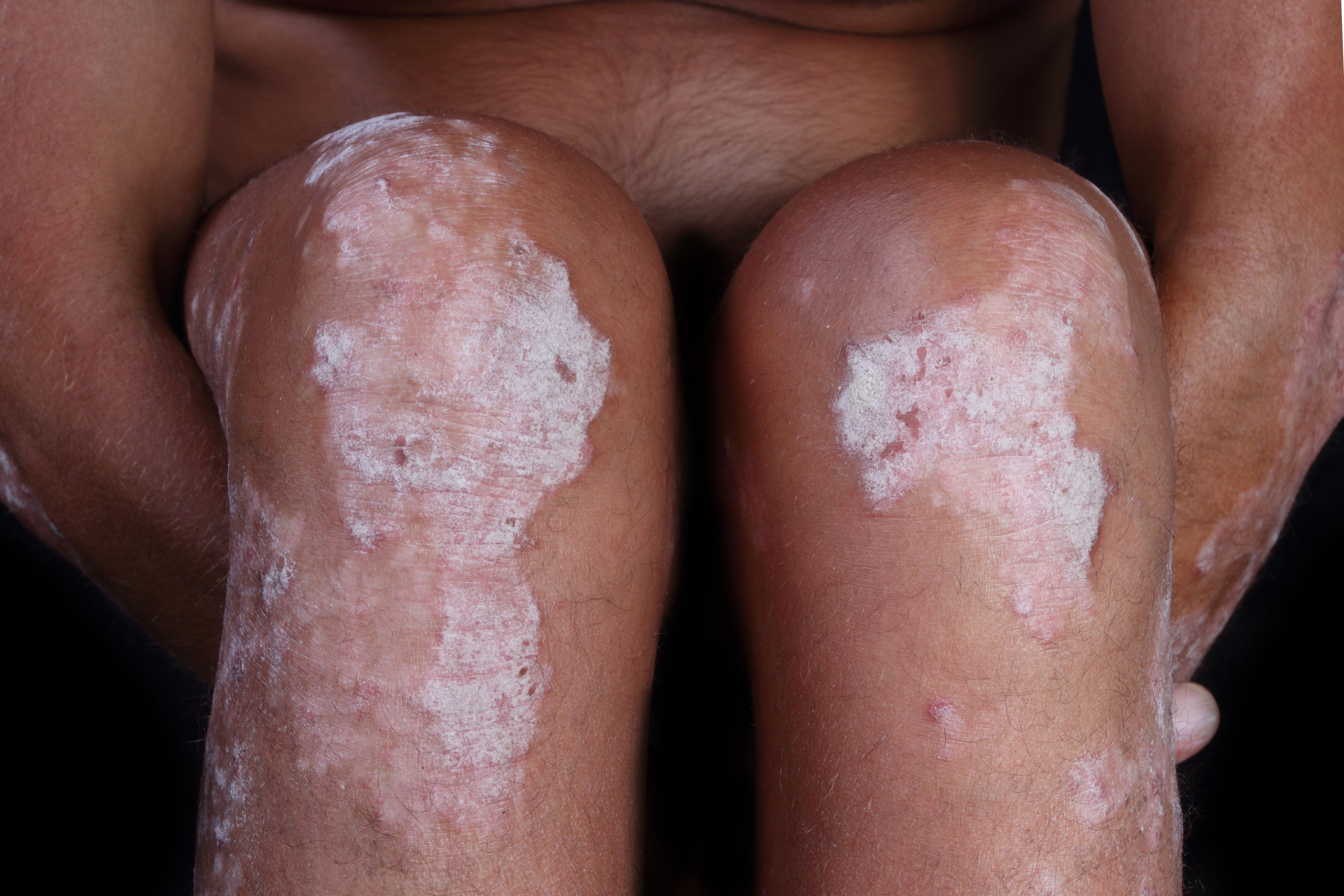
Topical halobetasol propionate 0.01% lotion appears to safely and quickly improve lower-extremity psoriatic lesions, according to a recent study.
“Past studies measuring changes in PASI scores have shown more rapid improvement of plaques involving the head and trunk compared to the lower extremities. This subgroup analysis demonstrated a reasonable and sustained response was achieved using halobetasol 0.01% lotion for lesions on the legs,” Dr. Bhatia says.
Dr. Bhatia

Topical halobetasol propionate 0.01% lotion (Bryhali, Bausch Health) appears to safely and quickly improve lower-extremity psoriatic lesions, according to findings reported recently in the Journal of Drugs in Dermatology.1
RELATED: Psoriasis cream safe, effective suggests EU phase 3 results
A post hoc analysis of data from phase 3 studies investigating the efficacy of halobetasol propionate 0.01% lotion for treating moderate-to-severe plaque psoriasis showed that the topical corticosteroid was associated with rapid improvement, and findings should help dermatologists with treatment decisions for patients with disease involving leg lesions, said Neal Bhatia, M.D., director of clinical dermatology at Therapeutics Clinical Research, San Diego, and the lead author of the paper.
At the end of the eight-week treatment period, rates of treatment success and overall treatment success were significantly higher for patients randomized to once-daily treatment with halobetasol 0.01% lotion compared with vehicle-treated controls (P<.001 for both comparisons).
“Many patients with psoriasis experience stubborn plaques on the legs,” Dr. Bhatia says. “Past studies measuring changes in PASI scores have shown more rapid improvement of plaques involving the head and trunk compared to the lower extremities. This subgroup analysis demonstrated a reasonable and sustained response was achieved using halobetasol 0.01% lotion for lesions on the legs.”
RELATED: Bimekizumab offers hope for skin clearance in psoriasis
It was encouraging to see that the logion was effective at improving disease on a larger, hair-bearing area of the skin, he adds.
“Traditionally, a lotion has not been the vehicle of choice for treating psoriasis given perceptions about penetration, but it might be preferred by patients over ointments or foams for use on the lower extremities.”
RELATED: IL-17 potential therapeutic target for pustular psoriasis
The analysis of adverse event data from the two phase 3 studies showed there were minimal safety concerns associated with the eight-week treatment course, he says.
“Potent topical corticosteroids are generally approved for use over two to four consecutive weeks because of safety issues,” he explains. “This lower concentration of a potent corticosteroid brings new flexibility and safety for longer treatment duration.”
STUDY DETAILS
The post hoc analysis included data from 234 participants in two multicenter, randomized, double- blind, vehicle-controlled studies. The subjects were randomized 2:1 to once-daily treatment. with halobetasol 0.01% lotion or vehicle. Treatment continued for eight weeks and patients were followed for four weeks thereafter.
The efficacy endpoints included treatment success, defined as a ≥2-grade improvement from baseline in individual signs of psoriasis (erythema, plaque elevation, and scaling) and overall treatment success, defined as a ≥2-grade improvement from baseline in the Investigator Global Assessment (IGA) score and a rating of “clear” or “almost clear.” The three psoriasis signs and IGA scores used a 5-point rating scale where 0=none and 4=severe.
RELATED: Socioeconomic factors affect psoriasis treatment outcomes
To be eligible for enrollment, patients had to have a score ≥2 for all three psoriasis signs, a score of 3 or 4 for at least two of the signs and a total score ≥8. In addition, they were required to have an IGA score of 3 or 4. Eligible patients also had to have an overall body surface area (BSA) ranging from ≥3% to 12%.
“The sample size and methods for assessment used in this study were appropriate for delivering the message about the value of this concentration of halobetasol,” Dr. Bhatia says.
RELATED: Phototherapy safe, effective for psoriasis
Mean size of the leg target lesion at baseline for the 234 patients was 42.0 cm2; 91% of the randomized patients completed the study. A statistically significant difference in treatment success rate favoring the halobetasol group over placebo was achieved by week four for all three psoriasis signs. At week eight, treatment success rates for improving erythema, plaque elevation, and scaling severity on the leg were 52.1%, 55,5%, and 58.2%, respectively, in the halobetasol group and 15.7%, 22.9%, and 22.2%, respectively, in the controls.
A statistically significant difference favoring halobetasol was also achieved by week four in the analysis of overall success rates. At week eight, the overall success rates in the halobetasol and control groups were 37.1% and 8.4%, respectively.
Efficacy was also evaluated by calculating an IGA x BSA composite score. Analyses showed that the mean percent change in the composite score was significantly greater in the halobetasol group compared with controls (50.5% vs 13.8%, P<0.001). In addition, a significantly higher proportion of halobetasol-treated patients achieved the composite score cutoff that defines a clinically meaningful effect (≥75% reduction from baseline; 37.7% vs. 7.2%, P<0.001).
RELATED: Considerations for psoriasis patients with skin of color
Patients also completed the 10-question Dermatology Life Quality Index (DLQI) at baseline and during follow-up. Corresponding with the improvements seen in disease severity, the DLQI results showed that by week 4, the halobetasoltreated patients achieved quality of life improvement that represents a clinically important difference. Mean DLQI score was improved further at week 8 in the halobetasol group, and at both visits, the improvement from baseline was significantly greater than in the control group. Â
Disclosures:
Dr. Bhatia is an advisor and/or investigator for Bausch Health.
References:
1. Bhatia ND, Vlahovic TC, Green LG, Martin G, Lin T. J Drugs Dermatol. 2019;18(10):1029-1036