- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Frontline Forum Part 1: Exploring Expert Perspectives on the Management of Acne Vulgaris
Author(s):
In part 1 of this Frontline Forum series, Neal Bhatia, MD; Dawn Eichenfield, MD, PhD; Lawrence Eichenfield, MD; Linda F. Stein Gold, MD; and Guy Webster, MD, PhD, discuss the practical and clinical considerations in the management of acne vulgaris, reviewing available treatment options and how to treat acne scars.
“The biggest cause of acne is puberty when sebaceous secretion animates, or androgen secretion animates the sebaceous gland, and triglyceride-rich sebum is produced. Propinibacterium acnes eats it and then becomes a target for inflammation,” explained Guy F. Webster, MD, PhD, the chief medical officer at NFlection Therapeutics and a clinical professor of dermatology at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia, Pennsylvania.
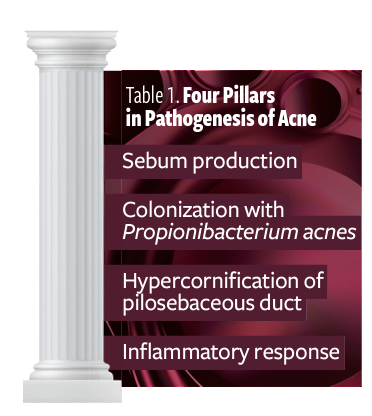
For panelist Linda F. Stein Gold, MD, considering and targeting the 4 pillars in the pathogenesis of acne (Table 1) is crucial when considering treatments for patients. Acne is often a generalized problem, added Stein Gold, director of dermatology clinical research and division head of dermatology at Henry Ford Health in Detroit, Michigan. “What I think is really important to remind everybody is that acne starts developing underneath the skin, so by the time you see the bump, there are probably 10 more bumps that are developing. We have to remember that this is more of a generalized…problem as opposed to that one pimple or papule.”1
Table 1
Assessing Severity
The panel agreed that assessing a patient’s acne severity is an important first step in addressing how to approach acne management. “It’s still something I’m very fascinated with—that I can look at someone’s face and not know if their chest and back is going to be totally covered or empty,” said Lawrence Eichenfield, MD, chief of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego, and moderator of the panel discussion.
“That’s true,” agreed panelist Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research in San Diego, California. “And you have to ask. If you don’t ask, you’re not going to see. But most [often the] assessment is in the first 5 seconds a patient walks in the door [and] you know how severe they are.”
Although Bhatia looks at skin picking as another indicator of severity, Stein Gold also looks at how acne presents on the patient. “Is this scarring acne? Is this acne that leads to permanent sequelae? A patient might be categorized as having mild acne, but we know that superficial acne lesions scar,” she said.
Quality-of-Life Impact
The panel agreed on the importance of discussing acne’s impact on a patient’s quality of life, no matter their age. Guy Webster explained, “Somebody with one nodule might say, ‘It’s nothing,’ and another person will say ‘It’s ruining my life’,” he said. “So, I lean more and more away from the research-y sort of evaluations and more say, ‘How bad is it bothering you?’ And then I’ll modify that by whether or not I think it’s scarring.”
“There’s a lot of joint decision-making with patients to try to figure out how much their acne is affecting their day-to-day lives and whether that 1 pimple is just devastating to them,” said Dawn Eichenfield, MD, PhD, an assistant clinical professor of dermatology and codirector of the Vascular Lesions Clinic at Rady Children’s Hospital-San Diego and the University of California, San Diego School of Medicine.
Discussing acne severity can be a difficult conversation with teenagers, but is important nonetheless, especially when parents do not want to be aggressive with treatment. The parents are usually the ones who prefer avoiding aggressive treatments, so Stein Gold tries to show them the increased anxiety caused by the acne. She noted that she asks her teen patients in front of their parents if they feel self-conscious at school due to their acne, to help emphasize the importance of treating this condition. She said, “This [acne] is affecting this child’s overall general sense of well-being.”
Managing Acne With Isotretinoin
The panelists noted that isotretinoin is often used as the first line of defense, but clinicians need to consider whether each patient is an immediate candidate. Stein Gold described the ideal candidate as having nodular cystic and widespread acne. Meanwhile, Dawn Eichenfield’sindication for isotretinoin is either moderate persistent acne or severe acne. Because of the medication’s adverse effects, monitoring patients who are prescribed isotretinoin for acne is an important consideration.2 However, there are misunderstandings that might lead dermatologists to dismiss its use, according to Bhatia. For instance, patients mistakenly believe they need to have laboratory work done every month and review symptoms, when in reality, that is not always the case. Nonetheless, caution is still important, he said. “You have to be thorough; you still must do the pregnancy test and follow the iPLEDGE [REMS (Risk Evaluation and Mitigation Strategy)] program, but not all the blood work. Those previous requirements were always a deterrent for many.”
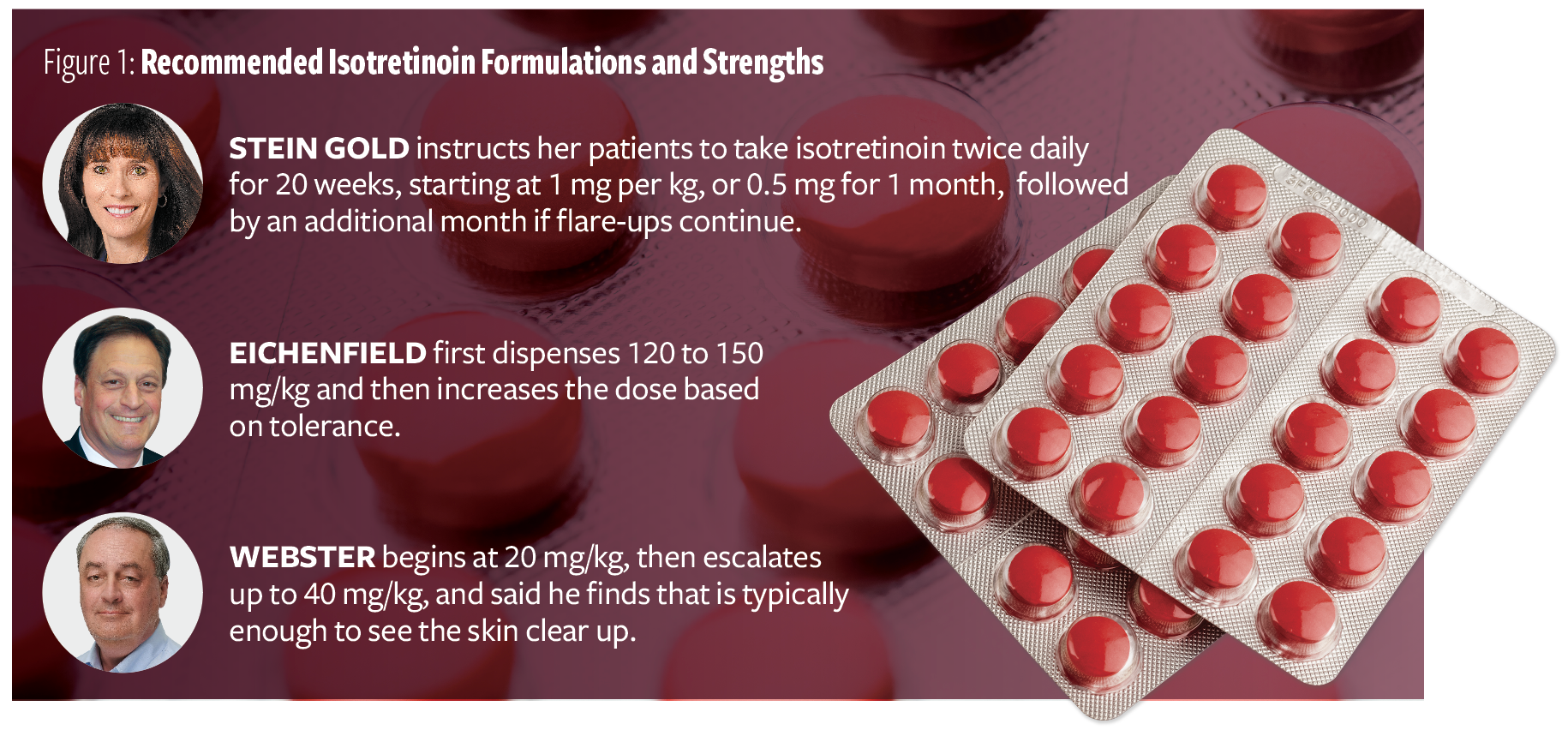
The panel also discussed the formulations and strengths of isotretinoin they prescribe (Figure 1).
Figure 1
Lawrence Eichenfield thinks most clinicians are comfortable using isotretinoin off label in patients without severe acne if they have not responded to other therapies and in patients with ongoing physical scarring.
The panel experts noted that the threshold to prescribe isotretinoin is lower now because patients are more conscious of the effects of antibiotics such as gastrointestinal upset, and many are hesitant to take more than 1 medication for a particular problem daily. The mixture of guideline recommendations and clinical practice experience has allowed clinicians “to become more comfortable with some of the [adverse] effect profile of isotretinoin that gave it a big stain,” Lawrence Eichenfield said.
Bhatia provides his patients with articles that discuss and educate patients on the adverse concerns related to isotretinoin use, many of which lack support.
Regardless of the safety profile, “Isotretinoin is disease-modifying,” Stein Gold said. “It is as close as we have to a cure for acne.”
Disclosure
This Frontline Forum is supported by Sun Pharmaceutical Industries Ltd.
References
1. Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945-973.e33. doi:10.1016/j.jaad.2015.12.037.
2. Bellomo R, Brunner M, Tadjally E. New formulations of isotretinoin for acne treatment: expanded options and clinical implications. J Clin Aesthet Dermatol. 2021;14(12 suppl 1):S18-S23.