
- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Find the Difference: Drug-Related Psoriasis
Author(s):
Lack of specific phenotypes complicates verification.
Drug-induced psoriasis from medications, including antimalarials or β-blockers, can be challenging to verify, according to Erik Stratman, MD, a medical dermatologist and chairman of dermatology at Marshfield Clinic Health System and former associate dean for the University of Wisconsin School of Medicine and Public Health—Marshfield Campus, both in Wisconsin.
Erik Stratman, MD

Therefore, learning which medications may induce or flare psoriasis can be important for accurate diagnosis and treatment, Stratman said in a presentation at the American Academy of Dermatology Virtual Meeting Experience 2021.1
Because no clear, specific phenotype distinguishes drug-induced psoriasis, Stratman pointed to the need to understand the 3 main types of reactions as a first step in determining whether medications provoked psoriasis induction or flare.
How to Assess Reactions
The first type of reaction occurs in a person with no history of disease who takes medicine and then experiences an onset of typical psoriasis. “If you are lucky enough to identify the drug and take the drug away, only sometimes will the psoriasis either substantially improve or disappear completely,” Stratman said. “In many cases, the psoriasis will persist.”
A second kind of reaction happens in a person with a history of psoriasis who, because of the drug, has a flare of existing psoriasis, such as worsening plaque or a more severe erythrodermic or pustular variant.
The third type of reaction occurs in a person with no history of psoriasis who takes a medicine, which results in a psoriasis-like reaction without necessarily having all the classic characteristics of psoriasis. “Often, when the drug is stopped, the reaction resolves in the weeks to months ahead,” Stratman said. “The reaction is not truly psoriasis, but rather psoriasiform in nature.”
Medications Most Likely to Impact Psoriasis
The association between drugs and psoriasis onset and/or exacerbation is difficult to attribute and study, according to Stratman. One reason is the frequently long, variable lag time with psoriasis induction or psoriasis flaring. “Usually flaring happens a little quicker than induction of new psoriasis from drug reactions,” he said. The lack of a specific phenotype for drug-related presentations further complicates the difficulties of establishing definite links.
In his experience, β-blockers are a key concern. “Perhaps we see more of this because of all the metabolic syndrome–related events we see with [patients with] psoriasis,” he said. “These patients are more likely to be prescribed β-blocker therapy.”
Sometimes a break from such treatment is a good starting point. “β-Blockers create not only new psoriasis but may flare existing psoriasis as well,” Stratman said. “In fact, β-blockers are probably the [most common] drug to trigger a new onset of psoriasis. Most of the other drugs cause flares of existing psoriasis.” (See Figure.1)
Figure.1
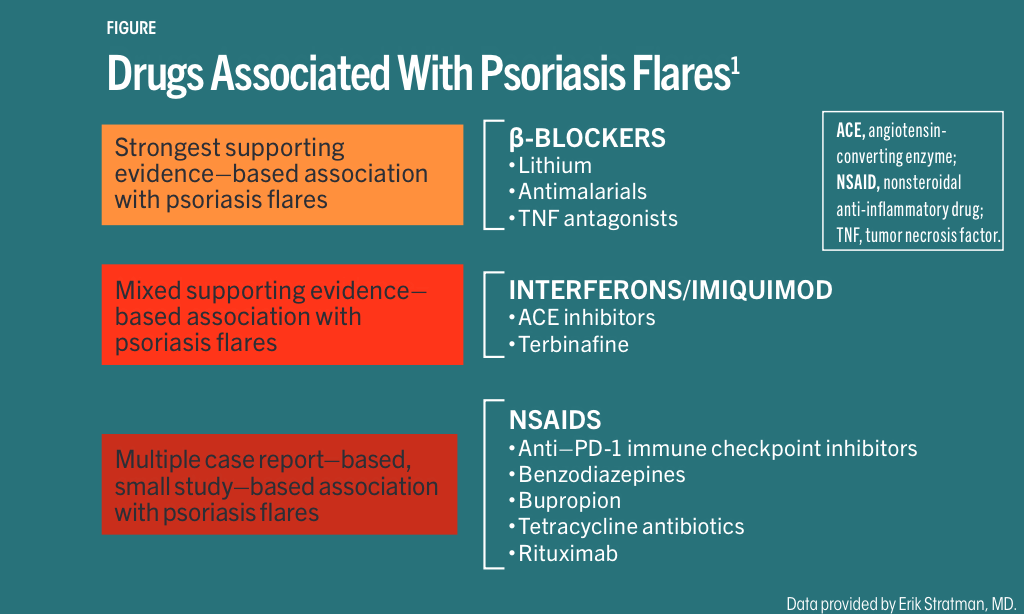
A large US prospective cohort study published in JAMA Dermatology in 2014 concluded that long-term regular β-blocker use for at least 6 years was linked to a 39% increased risk for psoriasis.2
On the other hand, lithium predominately exacerbates existing psoriasis, which can take up to 1 year to induce flaring, said Stratman.
Concerning antimalarials, hydroxychloroquine induces psoriasis more often than chloroquine, likely because the former is prescribed much more often and is more often associated with plaque flaring than new disease induction, Stratman added. Average time to flare is 4 to 12 weeks.
For erythrodermic and pustular flares with prednisone therapy, “in our textbooks, we are taught to avoid systemic steroids in [patients with psoriasis] because systemic steroids equal risk of psoriasis flaring,” Stratman said. “But this is counter to my clinical experience and research of others. Systemic corticosteroids are the No. 1 systemic agent prescribed for psoriasis therapy, eclipsing every biologic, methotrexate, and every systemic therapy.”
A recently published retrospective study in JAMA Dermatology conducted at rural Marshfield Clinic Health System found that the overall flare rate was only 1.42% among adult patients with a solid diagnosis of psoriasis who received at least 1 prescription course of a systemic corticosteroid for any reason and that a severe psoriasis flare occurred in only 0.07% of cases.3
The study population consisted of nearly 2000 patients approximately 50 years old (55% female) at the time of their first psoriasis diagnosis, followed by their first steroid prescription roughly 10 years later. Stratman added that 97% of steroid prescribing was done “outside of the field of dermatology” and that the most common steroid prescribed was prednisone.
Patients were seen at the facility at least once during therapy or within 3 months of stopping the medication (most commonly, oral prednisone) between October 2012 and July 2018.
Slightly more than 50% of patients had 1 steroid course, and 80% of the entire cohort had a total steroid course of less than 60 days. The median steroid dose was 40 mg.
A flare was defined by one of the following: a documented increase in body surface area; a higher Psoriasis Area and Severity Index score; the presence of pustular or erythrodermic skin; patient-subjective reporting of a worsening flare; a physical exam describing a worsening flare compared to a previous exam; or a provider assessment and plan that mentioned flare, rebound, or “objectively worse than before.”
“There was no difference in steroid dose between flaring patients and nonflaring patients,” Stratman noted.
The investigators identified a total of 16 flares among 516 manually abstracted patients. “However, 15 of the 16 patients had only worsening plaque-stage psoriasis,” Stratman said.
Of the 16 flares, 37% indicated flares that commenced prior to corticosteroids, and 18.8% were guttate flares with laboratory evidence of streptococcal pyogenes (strep throat) infection.
The sole erythrodermic patient was given systemic corticosteroids because of steadily worsening body redness. “I believe the flaring was already in motion rather than [being] caused by the steroid,” Stratman said.
“Our results suggest a very low rate of psoriasis flares [< 1.5%],” Stratman added. “We challenge the teaching/dogma that steroids induced [the] severe psoriasis flares in the general psoriasis population. Strict avoidance of systemic corticosteroids in [patients with psoriasis] may be unnecessary.”
However, Stratman listed some possible limitations of the study including:
- its retrospective nature;
- its use of only one large Midwest health care system;
- no control population of patients with psoriasis with no corticosteroid therapy;
- no previous use of criteria defining psoriasis flare;
- patient adherence to corticosteroid prescription; and
- patients may have received care outside of the system.
Despite the limitations, Stratman recommended that dermatologists consider the possibility of drug-induced psoriasis. “Do not overlook the medication list in [patients with] psoriasis,” he said.
Disclosure:
Stratman reported no relevant financial disclosures.
References:
1. Stratman, EJ. Does the use of systemic corticosteroids, antimalarials, or beta-blockers have an impact on patients with psoriasis? Presented at: American Academy of Dermatology Virtual Meeting Experience 2021; April 23-25, 2021. Accessed July 7, 2021.
2. Wu S, Han J, Li WQ, Qureshi AA. Hypertension, antihypertensive medication use, and risk of psoriasis. JAMA Dermatol. 2014;150(9):957-963. doi:10.1001/jamadermatol.2013.9957
3. Gregoire ARF, DeRuyter BK, Stratman. Psoriasis flares following systemic glucocorticoid exposure in patients with a history of psoriasis. JAMA Dermatol. 2021;157(2):198-201. doi:10.1001/jamadermatol.2020.4219
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.




