- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
A Close Look at Necrobiosis Lipoidica
Author(s):
How to diagnose and treat this rare skin disorder.
Necrobiosis Lipoidica (NL), also referred to as necrobiosis lipoidica diabeticorum, is a rare, inflammatory granulomatous disease, causing cutaneous collagen degeneration which increases the risk for ulceration of the skin, particularly after trauma.1-3 The disease is generally idiopathic, though it is traditionally associated with type 1 diabetes mellitus and cited to affect 0.3%-1.2% of pediatric diabetics.1,2
It classically presents as yellow-brown, atrophic, telangiectatic plaques with an elevated violaceous rim, classically on the pretibial surface. NL is typically chronic; most commonly occurring in women between the ages of 30 and 40 and is often associated with underlying autoimmune and inflammatory disorders. Skin biopsy revealing granulomatous inflammation, parallel collagen degeneration involving the entire dermis and extending into the subcutaneous fat, endothelial cell swelling, and thickening of the blood vessel walls should raise suspicion for this disease.
Clinical Presentation
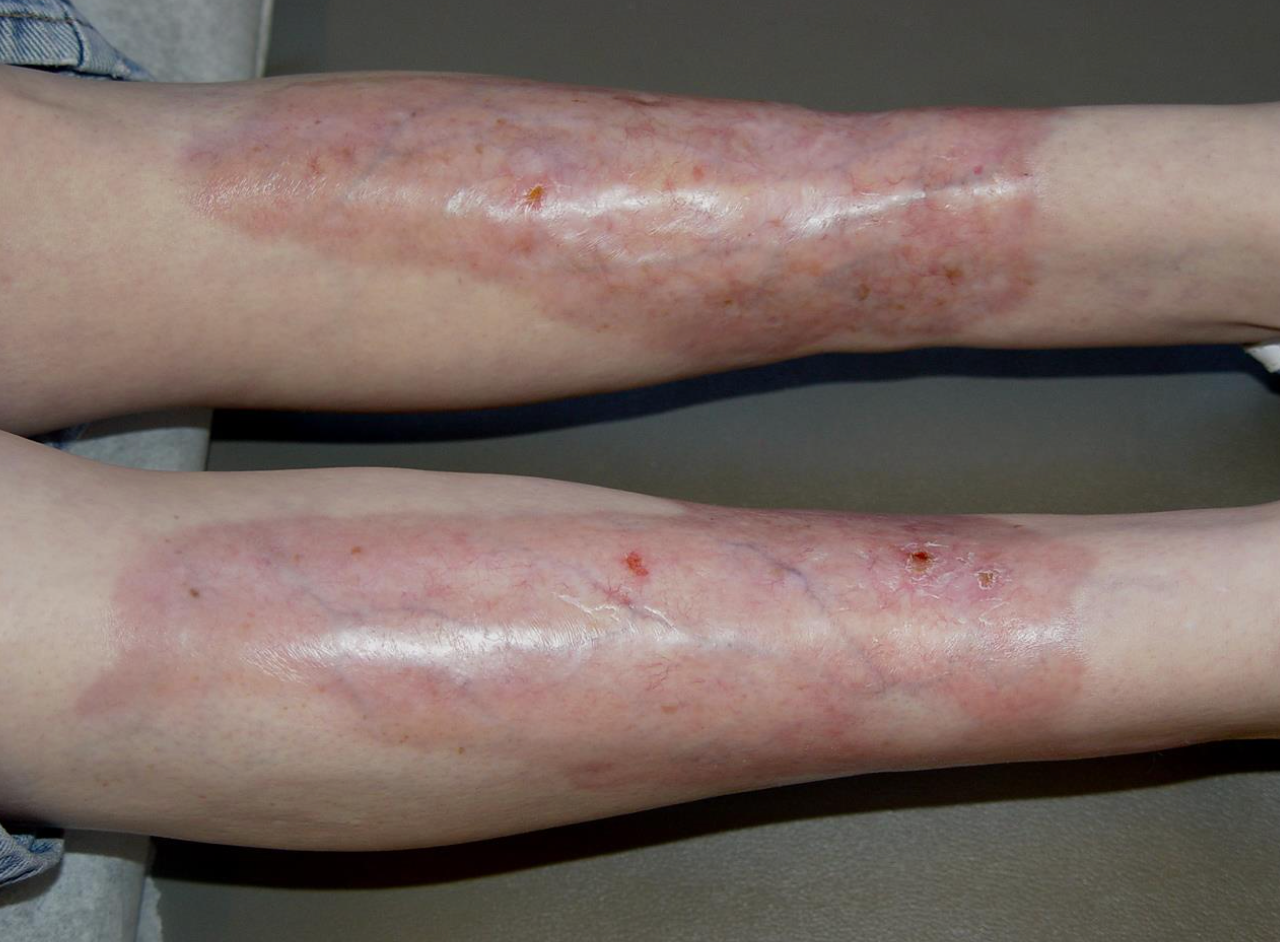
Skin lesions begin as 1- to 3-mm, well-demarcated papules that expand to become red-brown plaques with indurated borders and waxy centers (Figure 1). They later evolve into larger yellow-brown, shiny, atrophic, telangiectatic plaques with a violaceous rim (Figure 2). Central epidermal atrophy of the plaques increases the risk for ulceration. Ulceration occurs in roughly one- third of lesions, usually following minor trauma. Trauma can also cause the appearance of new skin lesions on previously unaffected skin or Koebner phenomenon. Lesions classically present on the pretibial surface, though lesions have been less commonly identified on the upper extremities, face, and scalp. The plaques are usually multiple and bilateral.
Figure 1: Annular pink-reddish plaques with central yellow-white portions and overlying telangiectasias and fine scale.

Etiology
The etiology of NL is largely unknown, though immune-mediated vascular disease is most widely accepted theory for the driver of this disorder.1-3 Common theories implicate immune complex deposition or microangiopathic changes as causes of vascular injury and subsequent collagen alteration. Still others attribute the development of NL to diabetic microangiopathy, immunoglobulins, complement, or fibrinogen deposition, abnormal collagen fibrils, impaired neutrophil migration, metabolic changes, or tumor necrosis factor-alpha.1,2 The tensile strength of collagen is depleted given the loss of the cross-striations of collagen fibrils.1 Defective neutrophil migration is a suspected cause of granuloma formation, as macrophages take on the neutrophil role and accumulate, with subsequent granuloma formation.
Figure 2: The bilateral shins with large, shiny, yellow-red confluent plaques with overlying telangiectasias, prominent veins, and few scattered erosions.
Risk Factors/Associated Disease
Though NL can occur in otherwise healthy individuals, there is an increased prevalence of disease among individuals with diabetes mellitus, particularly type 1.1- 4However, there is still debate regarding whether there is a relationship between glycemic control and risk of developing NL.1,5 Other comorbidities associated with NL include hypertension, hyperlipidemia, obesity, thyroid disorders, and inflammatory diseases, such as Crohn disease, ulcerative colitis, rheumatoid arthritis, and sarcoidosis.1,2,5
Diagnosis
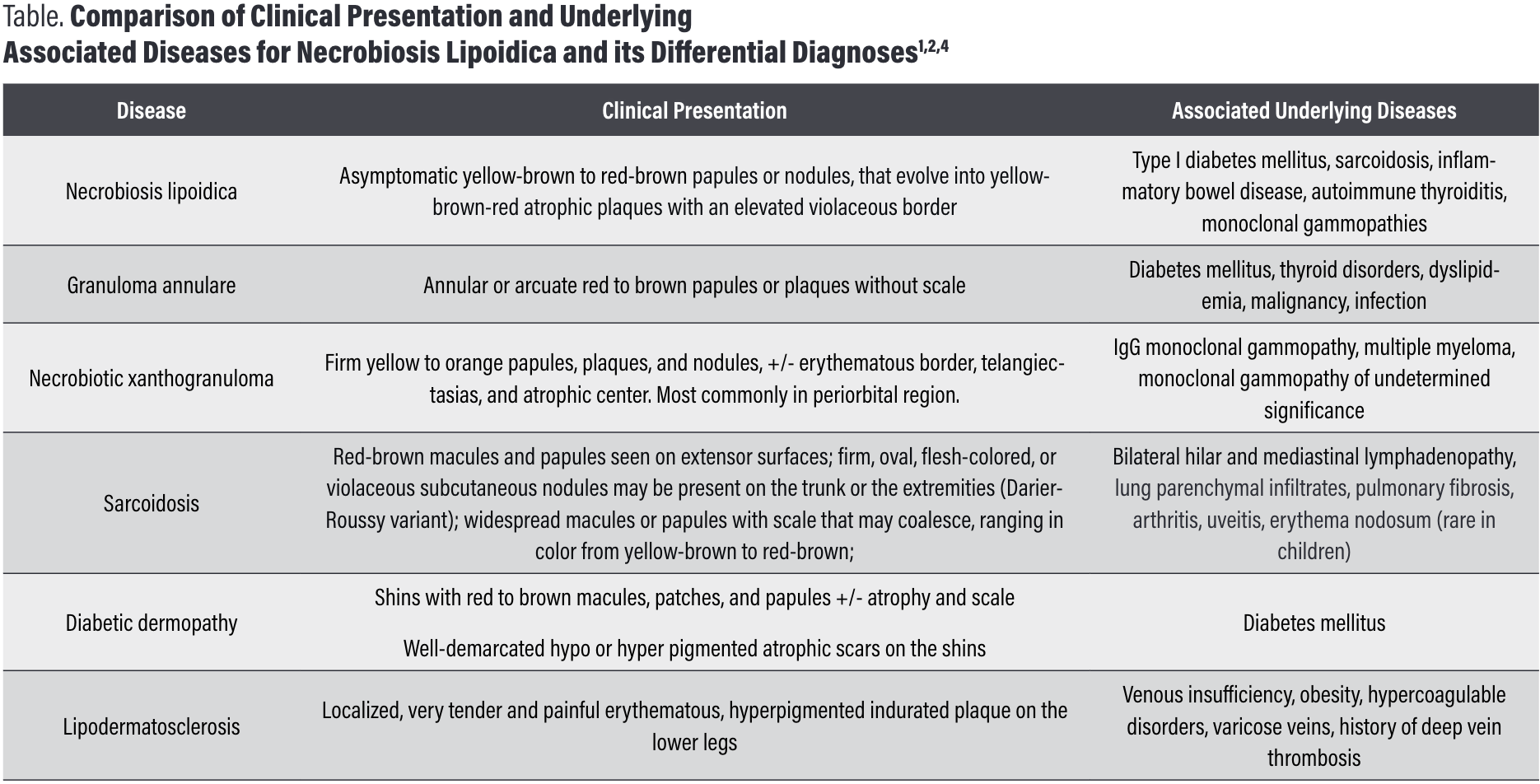
NL is primarily a clinical diagnosis; however, clinical suspicion often warrants a skin biopsy to rule out other similarly present-ing diseases, mainly granuloma annulare, necrobiotic xantho-granuloma, sarcoidosis, diabetic dermopathy, and Lipodermato-sclerosis (Table).1,2,4 Further, given its association with diabetes, obtaining baseline blood work including fasting blood glucose or glycosylated hemoglobin has become relatively standard.1
Histopathology
Histopathology reveals a normal or atrophic epidermis, with scattered palisaded and interstitial granulomatous dermatitis with layered tiers of granulomatous inflammation parallel to the skin surface, mixed with patches of collagen degeneration involving the entire dermis and extending into the subcutaneous fat septae.1,2 Endothelial cells characteristically reveal swelling and thickening of the blood vessel walls from the middle to deep dermis, which can also be found in diabetic microangiopathy.1
Management/Treatment
There is currently no standard treatment guideline for patients diagnosed with NL and it is rather difficult to treat. For early-stage lesions, first-line therapy typically includes potent topical corticosteroids.1- 4 Established lesions may benefit from intralesional corticosteroids injection into the active borders.1 For inactive, atrophic lesions, topical steroids should be avoided as they may exacerbate the atrophy and increase risk of ulceration. When ulcerations are present, proper wound care principles are important. UV light therapy, lasers, TNF-alpha inhibitors, calcineurin inhibitors, biologics, platelet inhibitors, surgery, and more recently JAK-inhibitors have also been trialed as treatment options for NL with varying results.1- 4,6
Treatment may provide intermittent disease quiescence, but since chronic in nature, its shows variable progression. Sites of previous ulceration or trauma are more susceptible to progressing to squamous cell carcinoma, and though this has been rarely reported, some argue for annual monitoring for transition to cancer following diagnosis.1,7 Ulcers can be painful, require extensive wound care, become infected, heal with scarring, and overall can significantly increase morbidity.1,3 Those with edema and associated venous disease of lymphedema may find compression therapy beneficial as adjunct treatment.
Table: Comparison of Clinical Presentation and Underlying Associated Diseases for Necrobiosis Lipoidica and its Differential Diagnoses1,2,4
References:
1. Lepe K, Riley CA, Salazar FJ. Necrobiosis Lipoidica. In: StatPearls. Treasure Island (FL); StatPearls Publishing; August 26, 2021.
2. Terziroli Beretta-Piccoli B, Mainetti C, Peeters MA, Laffitte E. Cutaneous Granulo-matosis: a Comprehensive Review. Clin Rev Allergy Immunol. 2018 Feb;54(1):131-146. doi: 10.10 07/s12016-017-8666-8
3. Rajabi-Estarabadi A, Aickara DJ, Hirsch M, Williams NM, Maranda EL, Van Badiavas E. Laser and light therapies for the treatment of necrobiosis lipoidica. Lasers Med Sci. 2021;36(3):497-506. doi: 10.10 07/s10103-020-03147-3
4. Reid SD, Ladizinski B, Lee K, Baibergenova A, Alavi A. Update on necrobiosis lipoidica: a review of etiology, diagnosis, and treatment options. J Am Acad Dermatol. 2013;69(5):783-791. doi: 10.1016/j.jaad.2013.05.034
5. Severson KJ, Patel MH, Brumfiel CM, Breen I, Butterfield RJ, Nelson SA, Sekulic A, Pittelkow MR, Mangold AR. Comorbidities and diabetic complications in patients with necrobiosis lipoidica. J Am Acad Dermatol. 2022;86(4):891-894. doi:10.1016/j.jaad.2021.03.026
6. Janßen S, Jansen TM. Ulcerated necrobiosis lipoidica successfully treated with tofacitinib. Int J Dermatol. 2022 Jun;61(6):739-741. doi: 10.1111/ijd.15960. Epub 2021 Nov 16. PMID: 34783006.
7. Harvey JA, Severson KJ, Brumfiel CM, Patel MH, Butterfield RJ, Nelson SA, Sekulic A, Pittelkow MR, Mangold AR. Necrobiosis lipoidica-associated cutaneous malignancy. J Am Acad Dermatol. 2022 Jun;86(6):1428-1429. doi:10.1016/j.jaad.2021.06.8 48







