- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Opinion
Article
Why AI is Not the Solution to All Dermatology Challenges
Author(s):
The integration of digital tools, including telemedicine, into routine clinical care is not without its hurdles.
Who is Danny/AdobeStock

In the vast expanse of modern healthcare, where technology and tradition intertwine, dermatology stands at a pivotal crossroads. The advent of artificial intelligence (AI) promises a revolution, yet its journey in dermatology is akin to navigating a labyrinth, filled with potential yet riddled with complexities. The promise of AI in dermatology is undeniably profound, ranging from enhancing electronic health records (EHRs) to revolutionizing diagnostic processes. However, the reality is a tapestry rich with challenges, demanding a nuanced understanding of AI's role in this specialty.
Digital health's emergence as a determinant of health underscores the significance of technological advancements in dermatology. The potential of AI in automating administrative processes, facilitating seamless communications, aiding in accurate diagnosis, and even powering advanced tools like dermoscopy for cancer detection is monumental. AI's role in discovering new treatments for chronic conditions like hidradenitis suppurativa, acne vulgaris, psoriasis, and atopic dermatitis cannot be overstated. Yet, the integration of these digital tools, including telemedicine, into routine clinical care is not without its hurdles.1
Dermatology's digital health landscape is, in many ways, still in its nascent stages. While AI brings the promise of transformative change, bridging the gap between potential and practical application remains a formidable challenge. The Organization for Economic Co-operation and Development (OECD) highlights a sobering reality: out of 38 countries, many struggle to extract maximum value from digital health due to outdated technologies and fragmented data environments. The healthcare sector, historically slower than others in leveraging digital transformation, saw a burst of change with the COVID-19 pandemic. Yet, significant barriers remain.2
Consider the reliance on archaic technologies like fax machines in healthcare, particularly in dermatology. Despite the evolution of communication technologies, an astonishing 75% of global fax traffic caters to medical services.3 This dependence not only impedes efficiency but also reflects a reluctance to embrace modern digital solutions. Furthermore, the lag between discovery and implementation is startling – with medical innovations taking an average of 17 years to become standard practice.4
The resistance to new technologies in healthcare, elucidated by Professor Michaela Kerrisey of Harvard Business School, is aptly described by the acronym RHIP – Risks, Habits, Identity, and Power. Each element, from perceived risks to identity symbols and power dynamics, forms a complex barrier to digital advancement. For example, the continued use of pagers in hospitals is not merely a technological choice but a cultural one, reflecting deeper aspects of medical practice and communication norms.5
The state of electronic health portals in dermatology presents another challenge. While most OECD countries have established such portals, less than half allow public access and interaction with comprehensive health data. This limitation not only restricts patient involvement in their care but also highlights a broader issue – the digital divide. For dermatology to fully harness AI's capabilities, a shift in mindset and practice is essential, one that transcends mere technological adoption.
Digital readiness in dermatology practices, a measure of the ability to effectively use analytics, data, and technology, is pivotal. Without this foundational readiness, the potential benefits of AI remain elusive. Dermatology practices must evaluate their digital infrastructure and strategies to improve skin health care effectively. This readiness is the cornerstone from which data can be leveraged for primary and secondary uses, enhancing individual and public health outcomes.2
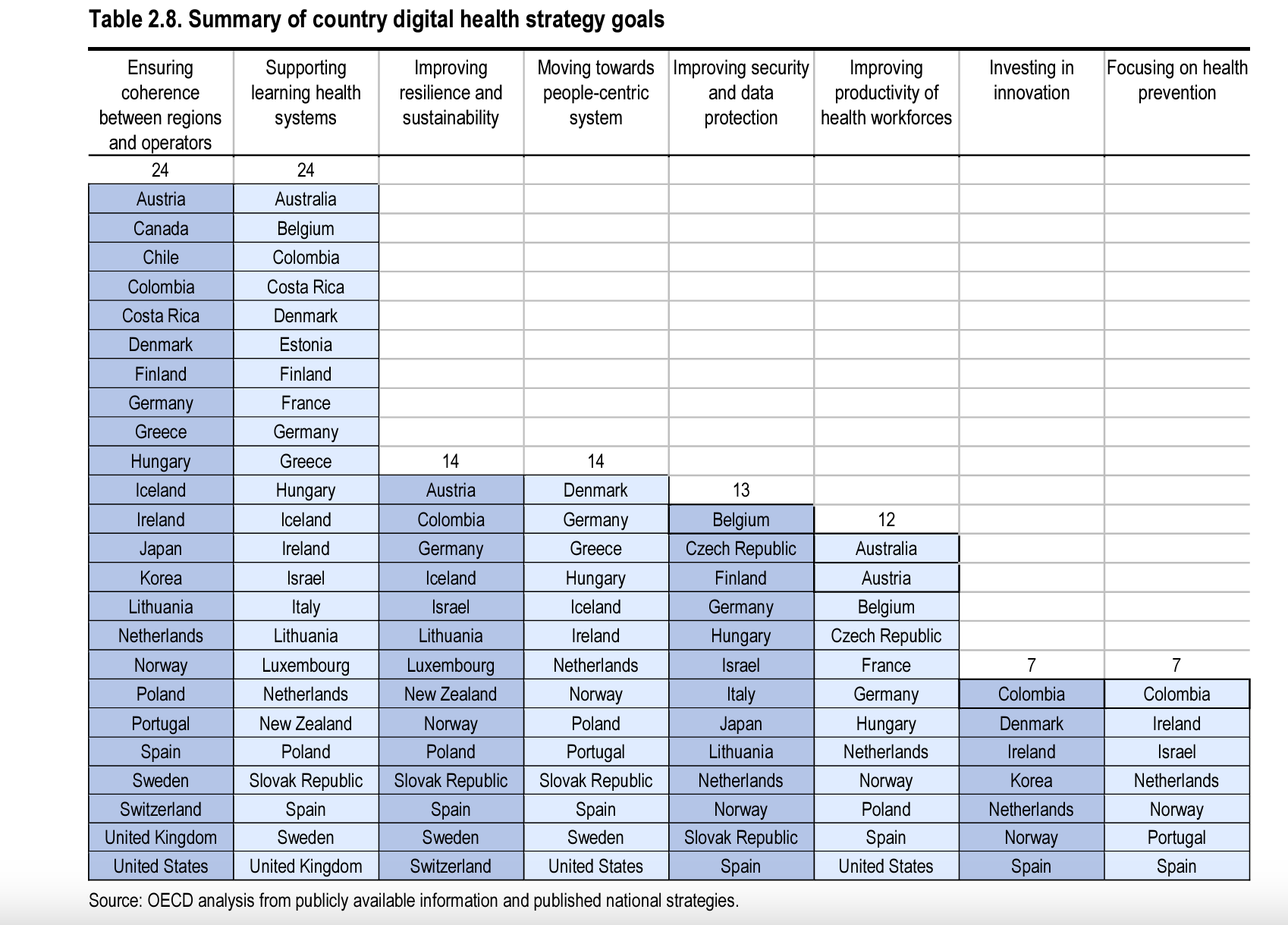
As illustrated in Table 2.8 from OECD’s “Health at a Glance: 2023,” a significant finding reveals that more than 70% of the OECD countries participating in the study have set specific objectives to bolster learning health systems. A 'learning health system' represents a methodology that emphasizes perpetual learning from each patient interaction and every aspect of healthcare delivery. This approach harnesses data and analytics to guide and enhance healthcare practices, policies, and outcomes. However, it's noteworthy that learning health systems are notably scarce across dermatology groups throughout the nation.1
Click to enlarge
Source: OCED. 2023. Summary of country digital health strategy goals. https://www.oecd-ilibrary.org/deliver/7a7afb35-en.pdf?itemId=%2Fcontent%2Fpublication%2F7a7afb35-en&mimeType=pdf
AI in dermatology, while a beacon of hope for improved care, is not a one-stop solution to the field's challenges. The journey to fully realize AI's potential involves addressing technological and cultural barriers, enhancing digital literacy, and building robust digital infrastructure. The future of dermatology in the digital age will be shaped not only by advancements in AI but also by the field's adaptability and willingness to embrace digital transformation.
The integration of AI in dermatology is not merely a technological leap; it's a cultural one. It requires an ecosystem where technology, practitioners, and patients coalesce harmoniously. Dermatology's journey with AI is a narrative of potential and caution, a story of innovation entwined with the legacy of traditional practices.
As we ponder the future of dermatology in this digital era, the role of AI looms large. Will dermatology practices rise to the challenge of bridging the digital divide and harnessing the power of AI? Or will they remain anchored in traditionalism, watching the digital revolution pass by? The answers to these questions will shape the trajectory of dermatology care, determining whether the field can fully unlock the transformative potential of AI.
In conclusion, AI in dermatology represents a complex interplay of innovation and tradition, potential and practicality. The path to harnessing its full potential is layered with technological, cultural, and systemic challenges. The future of dermatology in the digital age hinges on the field's ability to adapt, evolve, and embrace digital transformation. Only then can AI's true potential in dermatology be unlocked, ensuring that skin care, a vital aspect of healthcare, is elevated to new heights in the digital era.
Michael Rubio, PA-C, is a physician assistant at Infinity Dermatology in Brooklyn, NY. He is also the founder and Chief Product Officer of Plait (plaithealth.com), a patient service platform leading the way in digital transformation in dermatology practices nationally.
References
- What is a learning health system? Johns Hopkins Berman Institute of Bioethics. Accessed January 8, 2024. https://bioethics.jhu.edu/learning-health-systems/about/.
- OECD. Health at a glance 2023: OECD indicators. OECD Publishing; 2023. https://doi.org/10.1787/7a7afb35-en.
- The most surprising fax machine usage statistics and trends in 2023. Gintux. Updated December 25, 2023. Accessed January 8, 2024. https://blog.gitnux.com/faxmachine-usage-statistics/.
- Morris Z, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510-520. https://doi.org/10.1258/jrsm.2011.110180.
- Guo J, Fountain N, Romer K, Yellowhorse Kesler S. Why do doctors still use pagers? : Planet Money. NPR. Published December 8, 2023. Accessed January 8, 2024. https://www.npr.org/2023/12/08/1197955913/doctors-pagers-beepers.






