- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
Article
Triggering bullous pemphigoid
Author(s):
Scabies infection may be a trigger for bullous pemphigoid, and investigators plan to conduct a larger study to confirm their findings.

Key Points
National report - A scabies infection may predispose some patients to developing bullous pemphigoid (BP), according to research presented at the 2009 annual meeting of the Society for Investigative Dermatology.
Melanie Wong, B.S., one of the study's investigators, a medical student at the State University of New York (SUNY) Downstate Medical Center and a research fellow in the department of dermatology, University of Iowa, Iowa City, Iowa, notes that scabies infestations occur in an ordinary form in which there are fewer than 20 mites on the body, as well as in a crusted form, in which thousands to millions of mites are present.
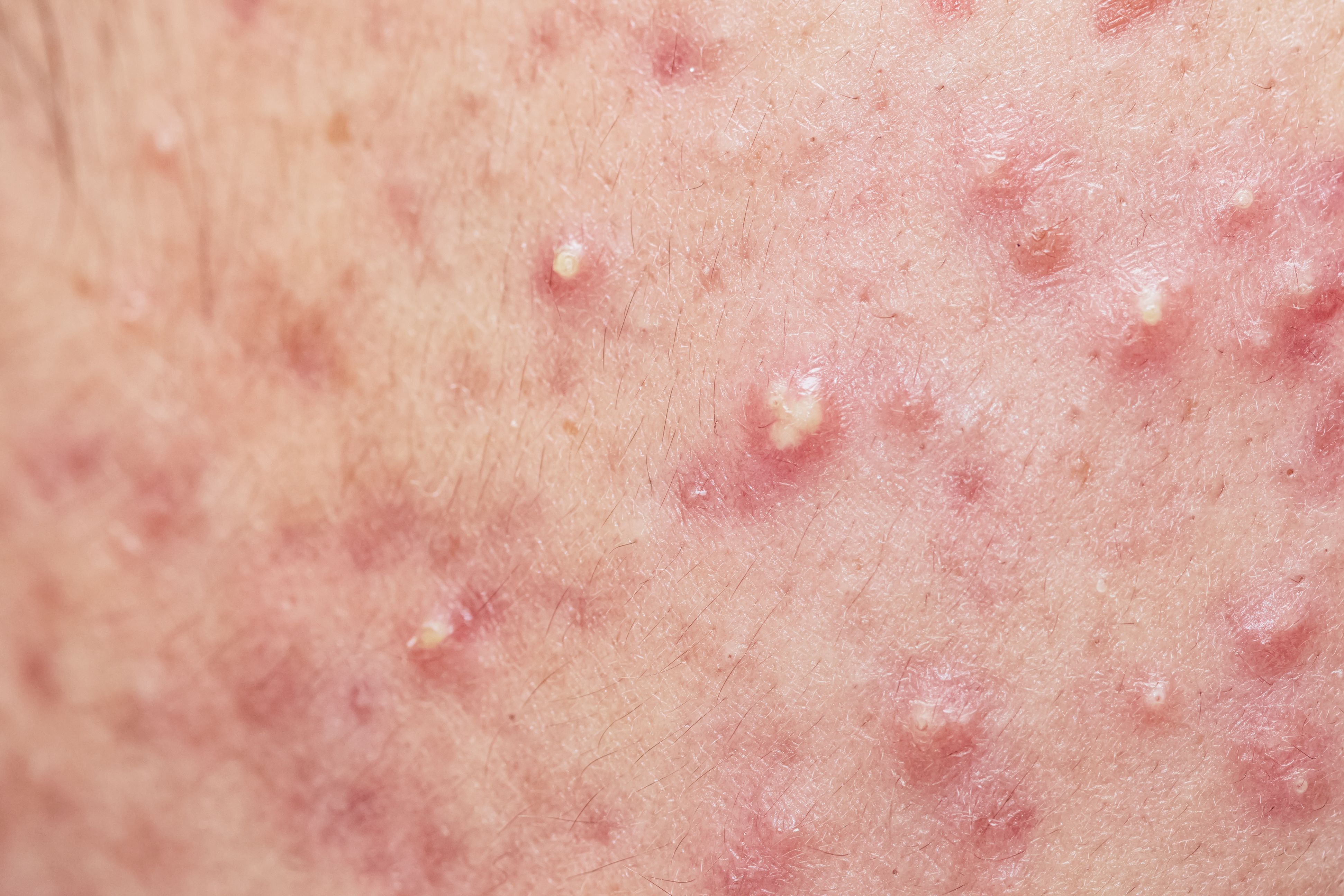
Scabies
Ms. Wong says BP is characterized by autoantibodies against the hemidesmosomal protein BP180.
"Because the diseases (bullous scabies and BP) look similar under the microscope and because there is subepidermal blistering with both, we were prompted to see if they (patients with scabies and bullous scabies) did produce cross-reacting autoantibodies to these proteins, which might cause the blistering," Ms. Wong says, noting that the initial immunologic trigger of BP remains unknown.
Protein similarities
Investigators observed three regions of similarity between BP230 and scabies proteins, and six regions between BP180 and scabies proteins, reflecting homology between BP proteins and scabies proteins, which suggests a role for molecular mimicry in triggering the production of cross-reacting autoantibodies.
Researchers collected blood samples from 17 patients who had ordinary scabies and 39 control patients. Investigators had access to archival sera from three patients with bullous scabies. The diagnosis of scabies was confirmed by the presence of a scabies mite on skin scraping. Investigators measured the levels of IgE antibodies and IgG BP180-specific and BP230-specific autoantibodies.
Study investigators also performed immunoblotting with an epidermal lysate and used bullous scabies sera to test for the presence of IgG antibodies to the skin. In addition, direct immunofluorescence was conducted on perilesional skin to determine basement membrane zone binding.
"We saw a significant elevation of BP180 IgG compared to controls," she says, noting that BP180 IgE and BP230 IgE, as well as IgG autoantibodies, were not elevated in a statistically significant way in scabies patients.
Ms. Wong says patients in this study who presented with scabies had a younger mean age, 44, while patients with bullous scabies had a mean age of 81, more closely resembling the mean age of patients with bullous pemphigoid, which is typically a disease of the elderly.
All three patients with bullous scabies, all of whom were positive for BP autoantibodies, were treated with scabicide. Two continued to have blistering despite the use of scabicide, suggesting that true bullous pemphigoid was present in those patients.
"We can say that they developed true bullous pemphigoid," Ms. Wong tells Dermatology Times. "It's interesting that we see a relationship between the two diseases and see that this (scabies infection) is perhaps a very rare trigger of BP."
In the future, researchers aim to confirm the results of this study by increasing the sample size of patients with scabies and looking for the presence of BP180 autoantibodies outside of a specific area of the protein, namely outside the immunodominant NC16A region, according to Ms. Wong.
Disclosure: Ms. Wong reports no relevant financial interests.