- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Article
Treating Skin Conditions in Asian Patients
Author(s):
Experts present detailed guidelines on how to diagnose and treat common skin diseases and conditions in the Asian American population.
Given the population growth among Asian Americans, dermatologists in the United States likely will be treating more patients from this diverse cultural community. Ensuring positive outcomes starts with understanding the differences in which skin conditions most commonly affect these patients and what that means for treatment regimens, according to an expert panel presentation at the American Academy of Dermatology Virtual Meeting Experience (AAD VMX) 2021, held in April.1
Asian Americans were the fastest-growing sector among all racial and ethnic groups in the United States between 2000 and 2019. The US Asian population grew 81% during that time, from approximately 10.5 million to a record 18.9 million. By 2060, the number of Asian Americans in the US is projected to surpass 46 million, according to the Pew Research Center.2
Learning to differentiate common and uncommon conditions is key to serving this expanding patient market, said AAD VMX session speaker Hye Jin Chung, MD, MMSc, assistant professor at Harvard Medical School and director of the Asian Skin Clinic at Beth Israel Deaconess Medical Center in Boston, Massachusetts. (Table 13).
Table 1
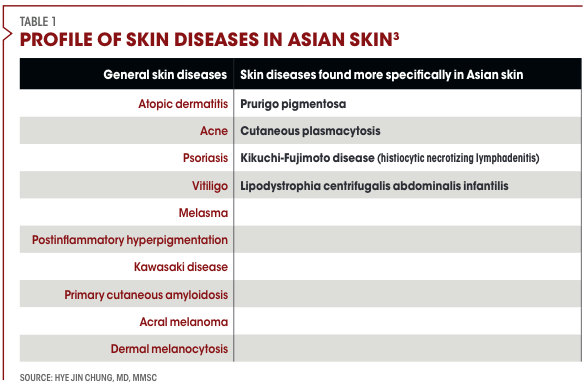
She outlined the 4 inflammatory disorders predominately found in Asian patients—prurigo pigmentosa, cutaneous plasmacytosis, Kikuchi-Fujimoto disease (also known as histiocytic necrotizing lymphadenitis), and lipodystrophia centrifugalis abdominalis infantilis—and offered strategies on how to optimize treatments for these patients.3
Prurigo Pigmentosa
Prurigo pigmentosa presents as recurrent, pruritic, erythematous papules with reticular pigmentation. “The main differential diagnosis for pruritic papules on the trunk of young people would be pityrosporum folliculitis,” she said. “But in pityrosporum folliculitis, the papules are all follicular centric and you do not see reticular postinflammatory hyperpigmentation.”
The early stage of prurigo pigmentosa is characterized by a superficial perivascular infiltrate of neutrophils, whereas spongiosis and necrotic keratinocytes often appear in later stages.3 “A definitive mechanism of pathogenesis has yet to be determined,” Chung said. “But its relationship with ketosis has been well documented. Prurigo pigmentosa is associated with anorexia nervosa, diabetes mellitus, strict ketogenic diet, and bariatric surgery.”
The “keto rash” has been reported in those on the ketogenic diet, which includes consuming high amount of fats and low amounts of carbohydrates. The new entity known as keto rash is actually prurigo pigmentosa, according to Chung, and now dermatologists are seeing patients with prurigo pigmentosa from other racial backgrounds.
“Prurigo pigmentosa is easy to treat with doxycycline or minocycline,” Chung said. “Topical steroids and antihistamines do not work.” Cases of prurigo pigmentosa linked to the ketogenic diet may resolve without medical intervention if patients increase their carbohydrate intake, she noted.
Cutaneous Plasmacytosis
Chung presented a case of a 68-year-old Vietnamese man with a rash on his trunk for more than 30 years. It began as pruritic but became asymptomatic. A punch biopsy on his back revealed dense perivascular and interstitial inflammation in the upper and middle dermis.
He received a diagnosis of cutaneous plasmacytosis, a benign proliferation of mature plasma cells. The pathogenesis is unknown, and it is common in middle-aged Asian individuals, she said.
Cutaneous plasmacytosis presents as skin lesions on the trunk, face, nape of the neck, and axilla as brown and red to purple-colored nonscaly patches, according to Chung.
There have been recent case reports of partial improvement with PUVA, a combination treatment consisting of prescribing the parent compound psoralen (P) and then exposing the skin to long-wave ultraviolet light (UVA) or excimer laser. Steroid injections, oral doxycycline, thalidomide, and chemoradiation have been used with little success, she added.
“Cutaneous plasmacytosis runs a chronic, largely benign course,” Chung said, noting that rare cases of cutaneous plasmacytosis have developed systemic involvement and clinicians should follow patients for malignancies and more.
Kikuchi-Fujimoto Disease
Kikuchi-Fujimoto disease presents with lymphadenopathy, fever, and erythematous macules with small central crusting on the head and neck. It is a rare benign condition that mimics tuberculosis lymphadenitis or lymphoma.
“Patients are generally younger than 40 years of age with female predominance. It is mainly described in Asia but also reported in America, Africa, and Europe,” Chung said.
Skin manifestation, or skin rash, has been reported in 10% to 40% of patients with Kikuchi-Fujimoto disease, she said. Signs and symptoms usually resolve within 1 to 4 months. Chung said dermatologists can treat these patients with more supportive measures, including analgesics, antipyretics, and rest. In more severe cases, she recommended that dermatologists consider short-course oral corticosteroids and/or hydroxychloroquine.
Although it is usually a self-remedying disease, it may recur in 3% to 4% of cases. Patients with Kikuchi-Fujimoto disease should be carefully monitored for development of systemic lupus erythematous, which has been associated with Kikuchi-Fujimoto, Chung advised.
Lipodystrophia Centrifugalis Abdominalis Infantilis
Authors of a statistical analysis of 168 cases of lipodystrophia centrifugalis abdominalis infantilis found that 160 were from Japan, South Korea, and China. The male-to-female ratio of cases was 1:1.6, and 80% of cases were on the groin, lumbar area, buttocks, or thighs.5
More than 90% of patients present by age 5, and mechanical irritation is the cause in only 10% of cases, according to Chung.
Although the lesions progress slowly over several years, Chung said spontaneous resolution has been observed in more than 50% of patients by the time they reach their teens.
“Topical tacrolimus and pimecrolimus have been reported to prevent enlargement of lesions,” she said. Chung added that chloroquine, penicillin, vitamin E, and ibuprofen, as well as topical therapies such as corticosteroids or vitamin A, can help treat the condition.
Differentiating Melanonychia from Nail Unit Melanoma
Treating Asian patients also requires in-depth knowledge of the differences in how skin disorders present. Mi Ryung Roh, MD, PhD, associate professor of dermatology at Yonsei University College of Medicine and head of dermatologic surgery at Gangnam Severance Hospital in Seoul, South Korea, detailed how to differentiate melanonychia, a common disorder in the Asian population, from nail unit melanoma.4
Table 2

“Longitudinal melanonychia is a longitudinally oriented brown-black band that extends from the matrix to the distal portion of the nail plate. It accounts for nearly half of the cases of chromonychia,” she said. “The most common cause of melanonychia in all morphologies is subungual hemorrhage, followed by nail matrix nevus and trauma.”
Nail unit melanoma, or subungual melanoma, is rare in Western countries, with a prevalence of 0.7% to 3.5% of all melanoma cases. In South Korea, Japan, and China, the prevalence is 10% to 25% of all melanoma cases. Peak incidence is in the fifth to seventh decade of age but can be diagnosed at a younger age. Thumb and great toe are common sites. Longitudinal melanonychia is the first manifestation in 38% to 76% of cases.6,7
Nail matrix biopsy is the recognized standard for diagnosing nail unit melanoma, but clinicians should consider biopsy-caused nail scarring and deformity, according to Roh.
Dermoscopic features favoring nail unit melanoma in longitudinal melanonychia include having a bandwidth percentage higher than 40% to 65%, multicolor features, granular pigmentation, subungual hyperkeratosis, and micro-Hutchinson sign.8
Longitudinal melanonychia caused by melanocytic activation commonly occurs in skin phototypes IV, V, and VI. Inflammatory disorders, including psoriasis, can activate longitudinal melanonychia, as can systemic disorders such as Addison disease. Trauma is also a common cause of melanocytic activation that causes longitudinal melanonychia, Roh said.
Iatrogenic factors, such as chemotherapeutic and other drugs, can cause melanonychia. Other causes include nutritional deficiency such as vitamin D deficiency, Roh said.
“Melanonychia is a challenging symptom for clinicians irrespective of the patient’s age,” she said. “With careful history, clinical examination, and dermoscopy it is possible to determine whether it is benign or malignant. In suspected cases, nail matrix biopsy must be performed [because] tissue diagnosis remains the gold standard for diagnosis.”
Diagnosing and Treating Common Facial Pigmentary Disorders
The 5 most common pigmentary concerns among Asian Americans are solar lentigines, melasma, acquired bilateral nevus of Ota-like macules, nevus of Ota, and postinflammatory hyperpigmentation, according to Woraphong Manuskiatti, MD, professor of dermatology at Siriraj Skin Laser Center at Mahidol University in Bangkok, Thailand.
Manuskiatti, who presented on common facial pigmentary disorders in Asians and their treatment at the virtual AAD meeting, said making the right diagnosis is the most important first step.9
“Solar lentigines present with multiple brown macules, mostly scattered all over the face,” he said.
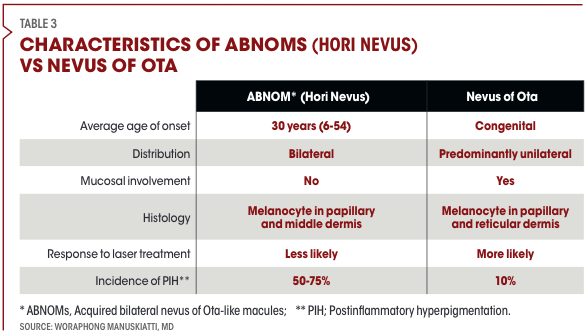
Although acquired bilateral nevus of Ota-like macules, or Hori’s nevus, is a similar condition to nevus of Ota, there are important differences. Average age of onset is 30, or between 6 and 54 years, for Hori’s nevus, whereas nevus of Ota is congenital. Hori’s nevus has a bilateral distribution vs a predominately unilateral distribution in nevus of Ota. There is no mucosal involvement in Hori’s nevus but there is in nevus of Ota.
Hori’s nevus histology features melanocytes in papillary and middle dermis versus melanocytes in papillary and reticular dermis for nevus of Ota. Hori’s nevus is less likely than nevus of Ota to respond to laser treatment, and the incidence of postinflammatory pigmentation is from 50% to 75% with Hori’s nevus compared with 10% in nevus of Ota, according to Manuskiatti (Table 3).
Table 3
Melasma, another common pigmentary disorder in Asia, presents as brown pigment distributed symmetrically around the face, usually on the forehead, bilateral cheeks, upper lid, chin, or nasal bridge.
Treatments vary according to the condition. For example, solar lentigines, acquired bilateral nevus of Ota-like macules (ABNOM or Hori’s nevus) and nevus of Ota can be treated with lasers. Melasma treatment usually begins with topicals, then chemical peeling and oral treatment, with lasers as an adjunct when needed. Postinflammatory hyperpigmentation is treated topically with oral therapy and laser as needed, according to Manuskiatti.
Manuskiatti presented a case of solar lentigines treated singularly with the Q-switched 532 nm Nd:YAG laser. Within 1 month, the patient was close to 100% improved. He also presented a patient with acquired bilateral nevus of Ota-like macules successfully treated 10 times with the Q-switched 1064 nm Nd:YAG laser, as well as a case of nevus of Ota 3 months after the eighth treatment with the 755 nm picosecond laser.
However, “melasma is still a headache for us,” he said.
First-line treatment for melasma includes tyrosinase inhibitors, hydroquinone, azelaic acid, kojic acid, arbutin, and licorice extracts. “Hydroquinone remains the most effective topical treatment for melasma, but no matter how effective it is a topical treatment alone does not produce impressive results in treating melasma,” Manuskiatti said. Studies have found that lasers should not be used as a first-line treatment for melasma but can be used as an adjunct in resistant cases.10
Manuskiatti said when he does use a laser to treat melasma, it is a low-fluence Er:YAG laser or 755-nm picosecond laser.
Authors of a retrospective study of 561 Asian patients with melasma treated for 4 months with oral tranexamic acid found nearly 90% improved, 10% did not improve, and 0.4% worsened. But the melasma often recurs after stopping the medication. In this study, 27.2% relapsed in a median 7 months.11
“Tranexamic acid may the game changer for treating melasma,” he said.
When treating postinflammatory hyperpigmentation, Manuskiatti starts with topical treatment.
“We also found the use of oral tranexamic acid is quite effective for treating postinflammatory hyperpigmentation. Pico toning [with the 755-nm picosecond laser] can be useful for treating laser-induced postinflammatory hyperpigmentation,” he said.
Disclosures:
Chung, Manuskiatti and Roh reported no relevant or financial disclosures.
References:
1. Chung HJ, Roh MR, Manuskiatti W. Skin Conditions in Asian patients that you do not want to miss: inflammatory diseases-1. Presented at: American Academy of Dermatology VMX; April 23-25, 2021; virtual.
2. U.S. Asian population grew fastest of any race, ethnicity in 2000-2019. Pew Research. Press release. April 9, 2021. Accessed May 6, 2021. U.S. Asian population grew fastest of any race, ethnicity in 2000-2019 | Pew Research Center
3. Beutler BD, Cohen PR, Lee RA. Prurigo pigmentosa: literature review. Am J Clin Dermatol. 2015;16(6):533-543. doi:10.1007/s40257-015-0154-4
4. Imamura S. Lipodystrophia centrifugalis abdominalis infantilis: statistical analysis of 168 cases. Pediatr Dermatol. 2012;29(4):437-441. doi:10.1111/j.1525-1470.2011.01584
5. Roh MR. Melanonychia vs nail unit melanoma. Presented at: American Academy of Dermatology VMX; April 23-25, 2021; virtual.
6. Singal A, Bisherwal K. Melanonychia: etiology, diagnosis, and treatment. Indian Dermatol Online J. 2020;11(1):1-11. doi:10.4103/idoj.IDOJ_167_19
7. Ko D, Oromendia C, Scher R, Lipner SR. Retrospective single-center study evaluating clinical and dermoscopic features of longitudinal melanonychia, ABCDEF criteria, and risk of malignancy. J Am Acad Dermatol. 2019;80(5):1272-1283. doi:10.1016/j.jaad.2018.08.033
8. Kungvalpivat P, Rojhirunsakool S, Chayavichitsilp P, Suchonwanit P, Wichayachakorn CT, Rutnin S. Clinical and onychoscopic features of benign and malignant conditions in longitudinal melanonychia in the Thai population: a comparative analysis. Clin Cosmet Investig Dermatol. 2020;13:857-865. doi:10.2147/CCID.S283112
9. Manuskiatti W. Common facial pigmentary disorders in Asians and their management. Presented at: American Academy of Dermatology VMX; April 23-25, 2021; virtual.
10. Sarkar R, Aurangabadkar S, Salim T, et al. Lasers in melasma: a review with consensus recommendations by Indian Pigmentary Expert Group. Indian J Dermatol. 2017;62(6):585-590. doi:10.4103/ijd.IJD_488_17
11. Lee HC, Thng TGS, Goh CL. Oral tranexamic acid (TA) in the treatment of melasma: a retrospective analysis. J Am Acad Dermatol. 2016;75(2):385-392. doi:10.1016/j.jaad.2016.03.001





