- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Article
Patients With Pressure Ulcers Face Compromised Skin Parameters
Author(s):
Such factors may include transepidermal water loss and skin barrier function.
Patients with pressure ulcers may also face several compromised skin parameters.
elkit/AdobeStock
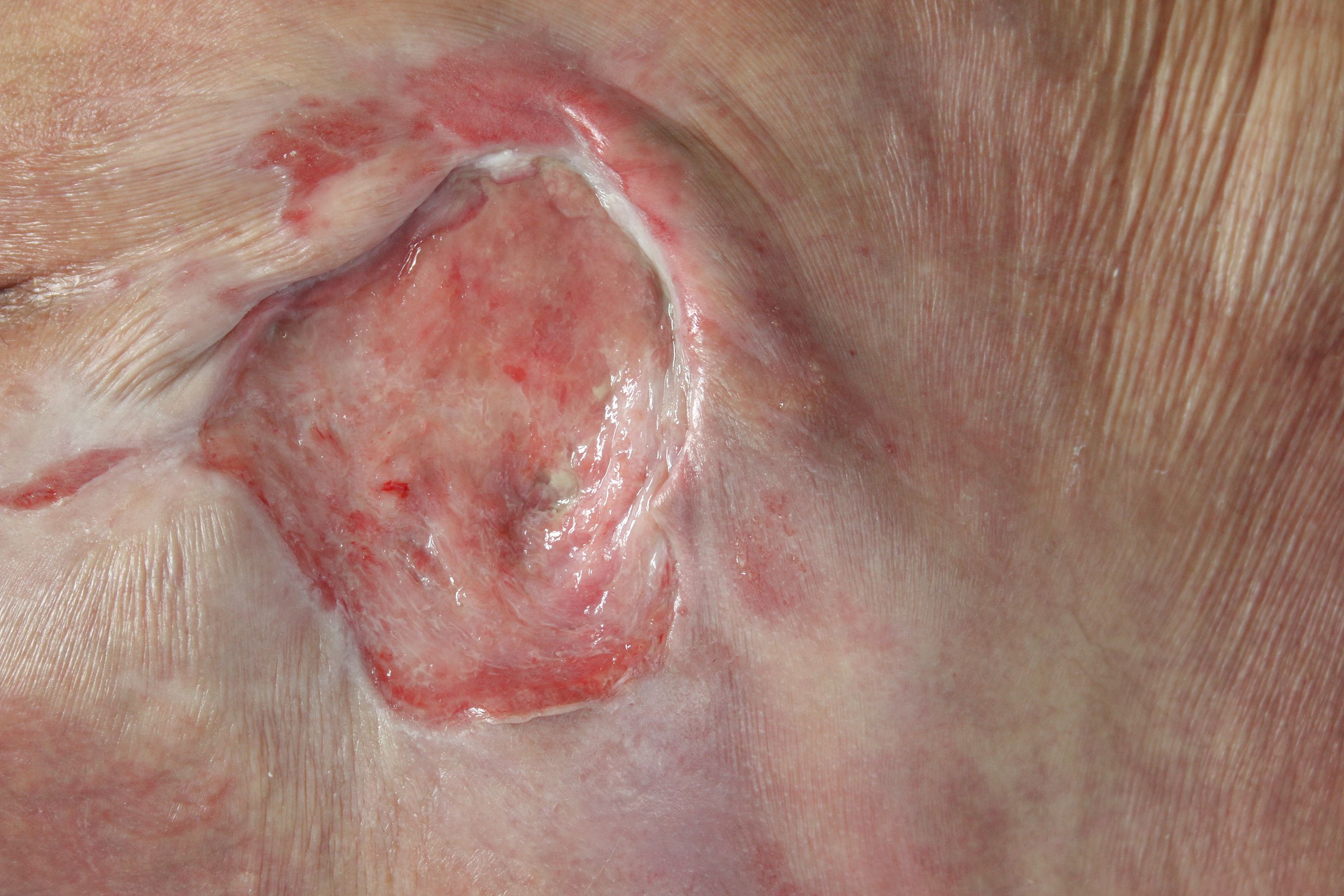
In a recent study,1 researchers sought to assess the ways in which a patient’s skin may be impacted by the chronic wounds, which can lead to a loss of skin integrity if not treated at an early stage. Furthermore, they cited existing research, including lab-based and dermatologic studies demonstrating biophysical skin parameters and skin health changes.
The study, which was observational, longitudinal, and cohort-involved in nature, began with a 4-month recruitment process of patients across 4 geriatric departments in the United Kingdom.
Prospective participants, of all genders and ethnicities, were expected to meet specific criteria, including being above the age of 18 and having a category I pressure ulcer. Potential participants were excluded from participation if they had existing skin conditions at the site of their ulcer, broken skin, or were unable to be repositioned due to medical reasons.
Additionally, all prospective participants presenting with redness were required to undergo a non-blanching erythema assessment and skin tolerance test.
Upon participant (n=30) selection, researchers recorded further relevant data, including skin damage descriptions, demographic data, skin care regimen, and measures adopted by physicians and care professionals in order to minimize patients’ risk or progression of skin damage.
Researchers collected data for 2 biophysical skin parameters: transepidermal water loss and stratum corneum hydration. These factors were assessed using a Tewameter TM 300 and a Corneometer CM 825 in 3 separate sessions. Participants’ risk of pressure ulcer progression was assessed using a risk assessment scale; all participants were those with a high risk of developing pressure ulcers.
Session 1 involved an initial skin assessment. At least 24 hours later, session 2 involved another skin assessment. At equal to or greater than 6 days later, session 3 involved a follow-up skin assessment.
“Data revealed that the TEWL [transepidermal water loss] values at the control site for all patients were at normative levels,ranging between 3.2 and 16.8 g/h/m2 and between 3.1 and 19.0 g/h/m2 on Sessions 1 and 2, respectively," study authors wrote. “By contrast, the corresponding TEWL values at the PU [pressure ulcer] sites ranged from 21.4 to 118 g/h/m2 and 18.4 to 157.5 g/h/m2. The differences in values between the two sites were statistically significant (P < .001), with a median difference between sites of 39.9 and 62.3 g/h/m2 on Sessions 1 and 2, respectively.”
While there were no clear or significant differences between stratum corneum hydration among control and pressure ulcer sites, researchers did note that some participants had higher skin hydration values or dry skin at pressure ulcer sites.
Researchers also conducted an analysis of several intrinsic factors, including anatomical location of the pressure ulcer, gender, mobility status, nutrition status, presence of diabetes, presence of incontinence, and previous history of pressure ulcers.
They noted significant differences in transepidermal water loss levels between genders, with female participants presenting with higher levels than male participants. These values were also higher in areas where pressure ulcers were located near the buttocks or sacrum, and in participants who were bedridden or experiencing incontinence.
In stratum corneum hydration levels, gender was again the main difference, with female participants experiencing higher levels. Participants’ mobility status and history of diabetes also significantly correlated with higher stratum corneum hydration.
“The present findings represent the first to present a correlation between two biophysical parameters, which was statistically significant for Session 2, for patients presenting with skin sites demonstrating a category I PU,” study authors wrote. “A similar correlation has been described previously in individuals affected by atopic dermatitis. Nonetheless, the present trend was not apparent for all participants in the cohort, with some demonstrating impaired barrier function (TEWL >50 g/h/m2) in dry skin.”
Reference
- Abiakam NS, Jayabal H, Filingeri D, Bader DL, Worsley PR. Spatial and temporal changes in biophysical skin parameters over a category I pressure ulcer. Internat Wound Journ. 2023. doi:10.1111/iwj.14194






