- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
News
Article
Image IQ: Inflammatory bowel disease with a deep pustule on the leg
Author(s):
Image IQ: A 55-year-old woman with a history of inflammatory bowel disease reported a very painful, deep pustule on her leg that may rupture. What’s your diagnosis?
Image IQ: A 55-year-old woman with a history of inflammatory bowel disease reported a very painful, deep pustule on her leg that may rupture. What’s your diagnosis? (Photo courtesy of VisualDx 2018)
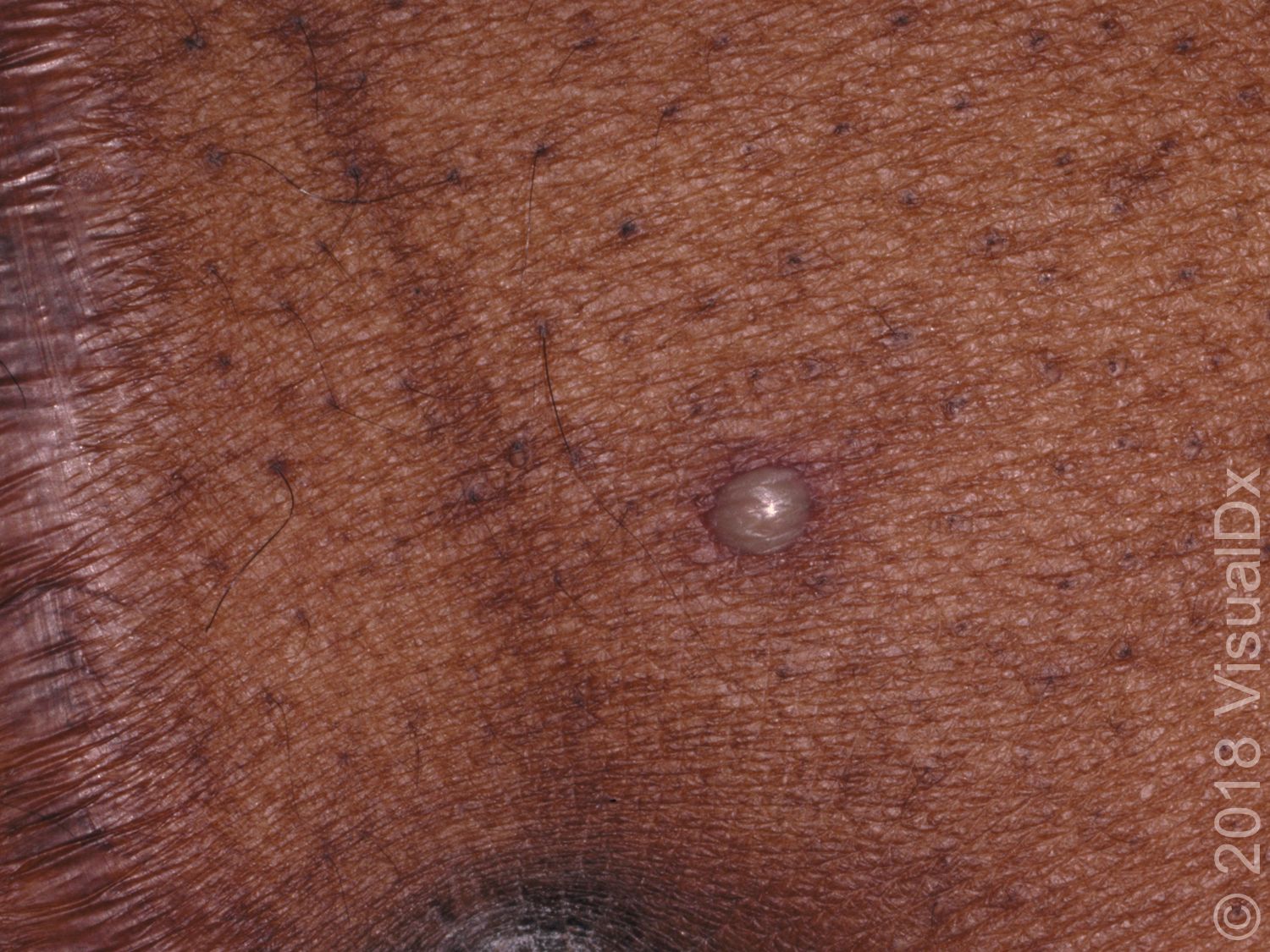
A 55-year-old woman with a history of inflammatory bowel disease reported a very painful, deep-seated pustule on her leg that looked like it might rupture. She also had a fever and some arthralgia, but she wasn’t sure if they were related.
What’s your diagnosis?
A. Furunculosis
B. Cellulitis
C. CA-MRSA skin infection
D. Pyoderma gangrenosum
Click on the next page for the answer.
The correct answer is D: Pyoderma gangrenosum
Pyoderma gangrenosum (PG) is an inflammatory, noninfectious, ulcerative neutrophilic skin disease of uncertain etiology commonly misdiagnosed as an aggressive skin infection. Pustules form and give way to ulcers with a necrotic, undermined margin. PG can affect any age and take on a number of differing clinical presentations. PG can have either an acute or chronic course and result in extensive scarring (which can be keloidal or have dyspigmentation, especially in patients with darker skin types). There is no predilection for sex or any population. The disease occurs most often in middle-aged adults.
The two primary variants are a classic ulcerative form, which often involves the lower extremities, and a vesicobullous form, which is more superficial and tends to occur on the upper extremities, including hands. Fever, toxicity, and pain can be associated with the onset of PG. Rarely, PG can involve the eyes as well. Extracutaneous manifestations may take the form of sterile neutrophilic abscesses, such as in the lungs, heart, gastrointestinal tract, liver, eyes, central nervous system, and lymphatic tissue.
Though the exact cause is unknown, neutrophil dysfunction, inflammation, and genetics are all thought to play a role. Additionally, PG has associations with a number of systemic illnesses. In about 50% of cases, there is an association between PG and systemic diseases such as ulcerative colitis, Crohn disease, arthritis, myeloma, leukemia, monoclonal gammopathy, granulomatosis with polyangiitis (formerly known as Wegener granulomatosis), collagen vascular disease, metabolic syndrome, and Behçet disease, among other disorders. Surgery by itself can be a precipitating cause. Levamisole-contaminated cocaine has been associated with PG lesions ranging from vesicopustules to bullae to larger ulcers; most patients demonstrated positivity for antiphospholipid or anticardiolipin antibodies.
PG tends to be self-limited. First-line therapies are widely accepted, while alternative therapeutic recommendations are largely based on anecdotal evidence. Surgical intervention is a common exacerbating factor because PG demonstrates pathergy, a phenomenon by which skin trauma can lead to worsening disease.
ICD 10 Code: L88 – Pyoderma gangrenosum
For more information about this quiz â specifically, differential diagnoses and pitfalls, clinical tests, management pearls, therapy and a complete list of references â visit VisualDx online.






