- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Article
HPV vaccine possibly linked to cutaneous PAN
Author(s):
The first documented case of cutaneous polyarteritis nodosum following HPV vaccine injection suggests dermatologists should consider it as a possible vaccine-related complication, says a pathologist who worked on this case.
Warwick, Rhode Island - A case study documenting the first instance of cutaneous polyarteritis nodosa (PAN) following Gardasil vaccination (human papillomavirus quadrivalent (types 6, 11, 16 and 18) vaccine, recombinant; Merck) suggests that this disease should perhaps be listed as a rare but serious complication of the vaccine, says a pathologist who worked on the case.
In late 2007, a 19-year-old female presented at an outpatient dermatology practice (affiliated with the Department of Dermatology at the Warren Alpert Medical School of Brown University) based in Warwick, Rhode Island, four weeks after receiving her first dose of Gardasil, says Leslie Robinson-Bostom, M.D., associate professor of dermatology, Warren Alpert Medical School of Brown University. The patient's symptoms included multiple 1 cm to 2 cm pink tender nodules on her lower extremities and dorsal upper extremities, as well as associated lower extremity swelling, joint pain and muscle aches.
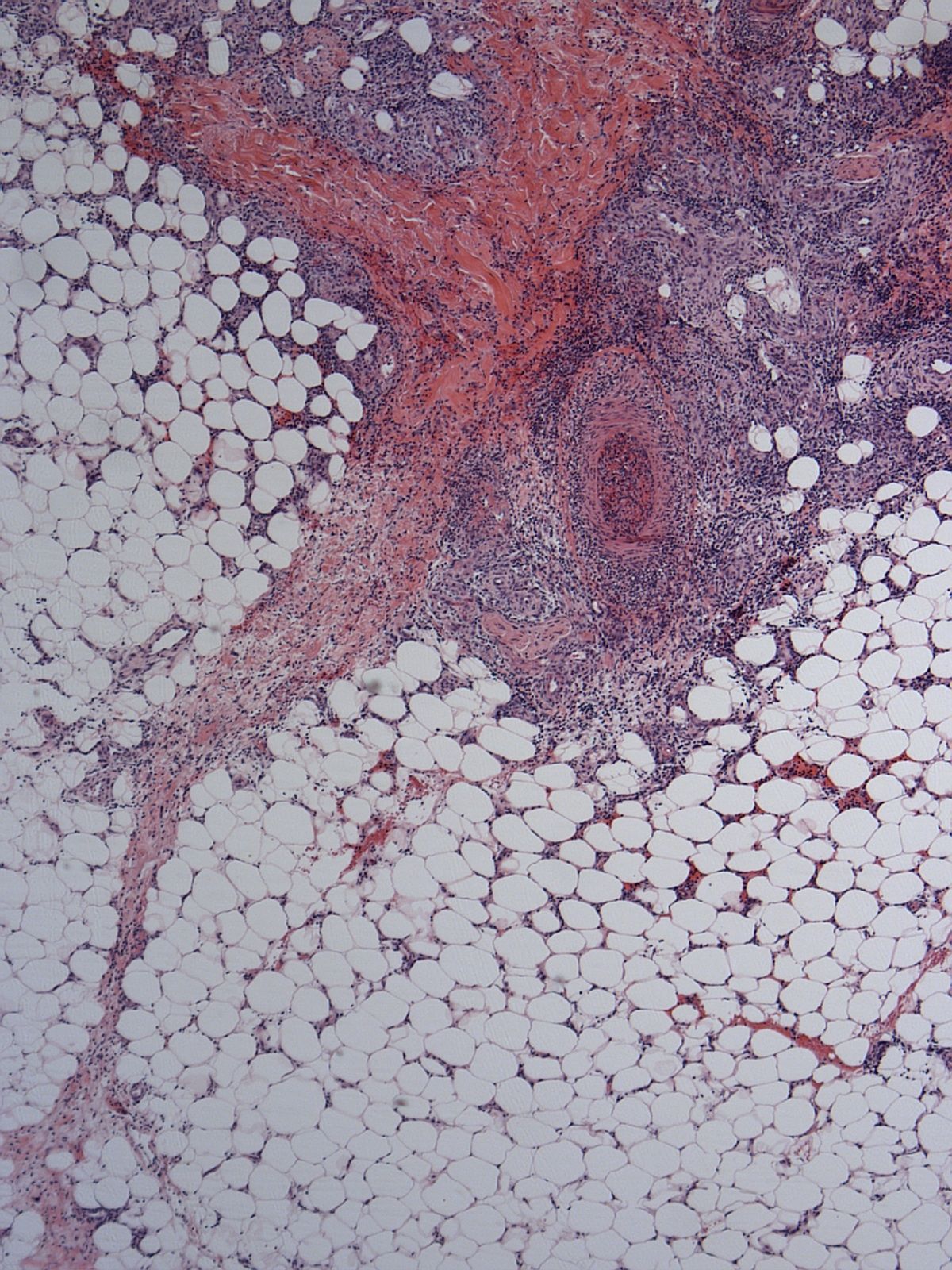
Histologic image showing thrombosed artery in 19-year-old female patient. Photo: Leslie Robinson-Bostom, M.D.
After clinically and histologically analyzing the patient, the dermatologists who treated her, led by Paula Moskowitz, M.D., Ph.D., determined that her symptoms were consistent with cutaneous PAN. More specifically, Dr. Robinson-Bostom says extensive laboratory and radiologic testing uncovered an elevated erythrocyte sedimentation rate of 73. Additionally, a punch biopsy taken from the patient's left calf revealed a deep dermal artery with luminal thrombosis, numerous neutrophils and dense surrounding mixed inflammation. This inflammation included primarily neutrophils, along with lymphocytes, eosinophils, histiocytosis and mast cells.
Furthermore, a clinical exam performed 12 weeks after the patient first presented uncovered asymptomatic, linear, stellate, pink to brown hyperpigmented plaques overlying the vessels on the interior lower extremities below both knees forming a livedo racemosa pattern, Dr. Robinson-Bostom says.

View from clinical exam 12 weeks after presentation showing linear pink to brown hyperpigmentation plaques forming a livedo racemosa pattern. Photo: Leslie Robinson-Bostom, M.D.
"When she initially presented to the dermatologist," she states, "her lesions clinically looked more like erythema nodosum. But subsequently, she developed more of a livedo pattern, which is more consistent with PAN, although one can see nodules in PAN as well."
Seeing thrombosis of the medium-sized artery in the deep dermis with numerous neutrophils and surrounding mixed inflammation on biopsy clinched the diagnosis, she adds.
Physicians treated the patient with saturated solution of potassium iodide (SSKI), and her lesions cleared, Dr. Robinson-Bostom says. "She is doing very well and opted not to receive another vaccination."
Medical literature includes five reports of vasculitis associated with the HPV vaccine. "But PAN hadn't been previously reported," she says.
This solitary case report of a patient who developed cutaneous PAN after receiving her first Gardasil dose could represent a coincidence, or perhaps another side effect from the vaccine, Dr. Robinson-Bostom says.
Other potential confounding factors include the fact that the patient was taking oral contraceptives and discontinued them when her symptoms appeared, she says. "Oral contraceptives can be associated with vasculitis, including PAN."
Physicians also know that the hepatitis B vaccine is associated with development of cutaneous PAN, but usually this occurs after the second dose, Dr. Robinson-Bostom says.
In some cases of cutaneous PAN, she says, "It's an immune complex mediated disorder that appears after multiple exposures to a vaccine."
Since the patient developed these lesions after only one exposure to the HPV vaccine, Dr. Robinson-Bostom says, "Perhaps she had been previously exposed to the HPV. But unfortunately, we don't have proof of that."
If the patient had no previous HPV exposure, Dr. Robinson-Bostom says, "We're not aware of any mechanism by which she would develop these lesions."
To detect this possible complication of the HPV vaccine clinically, she recommends that dermatologists look for nodules, ulcerations, a livedo pattern and perhaps hemorrhagic necrosis in patients who are undergoing or have undergone HPV vaccination.DT
Disclosure: Dr. Robinson-Bostom reports no relevant financial interests.
For more information
www.aad.org
www.lifespan.org






