- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
Article
Ethnic pigmentary disorders can be tricky to diagnose
Seattle - In the United States, there are very fewdermatologists who consider disorders of pigmentation to be a majorfocus of their practices and, as a result, they are more likely toresort to biopsy than they are to clinical criteria for makingthese diagnoses, according to Philip E. LeBoit, M.D., adermatopathologist and professor of clinical pathology anddermatology, University of California, San Francisco.
Seattle - In the United States, there are very few dermatologists who consider disorders of pigmentation to be a major focus of their practices and, as a result, they are more likely to resort to biopsy than they are to clinical criteria for making these diagnoses, according to Philip E. LeBoit, M.D., a dermatopathologist and professor of clinical pathology and dermatology, University of California, San Francisco.
"Pigmentary disorders can adversely affect people's lives. In India, for example, one of the most common pigmentary disorders, vitiligo, is often confused with leprosy and can lead to a stigma not just on the individual who has it but, also, on the individual's entire family," Dr. LeBoit says. "It is factors like those that make accurate recognition and treatment of disorders of pigmentation very important."
In the past, dermatopathologists studied disorders of pigmentation using such tools as DOPA stains on sheets of detached epidermal cells and by electron microscopy. But they no longer use those two techniques for practical diagnosis, according to Dr. LeBoit.
"We use predominately routine hematoxylin and eosin (H&E) staining, as well as immunoperoxidase staining, to make pigmentation disorder diagnoses today," he says.
Vitiligo
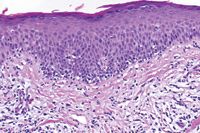
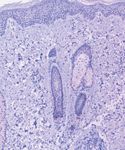
"The most striking change in vitiligo is an absence of melanocytes in the basal layer of the epidermis," he says. "In the past, electron microscopy and, later, staining with S100 protein was used. The S100 stain was not particularly good at labeling epidermal melanocytes and also stained Langerhans cells. So, the approach has been supplanted by Melan-A or MART-1, two similar monoclonal antibodies. Either one of these stains in a fully developed lesion of vitiligo will confirm absence of melanocytes."
An often misunderstood histopathologic aspect of vitiligo is that the early inflammatory lesions have more lymphocytes in them than was previously thought and, for that reason, can be confused with hypopigmented mycosis fungoides.
"This is also the case with the edges of lesions in trichrome vitiligo," he says.
Hypopigmented mycosis fungoides
Dermatologists in the United States often misdiagnose the somewhat rare pigmentary disorder hypopigmented mycosis fungoides.
"In particular, hypopigmented mycosis fungoides is often seen in children. It is much more common for mycosis fungoides, in general, to present in middle aged or in older patients, so many clinicians are not thinking about it when they see a child or teenager with areas of hypopigmented skin," Dr. LeBoit says.
Unlike vitiligo, the hypopigmented lesions are not clinically symmetrical and often do not have a sharp border. The changes on biopsy that one sees in hypopigmented mycosis fungoides are often subtle.






