- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
Article
Diagnostic techniques for desmoplastic melanoma
Diagnosing challenging melanocytic lesions typically requires combining immunostains-such as S100 and P16-with the dermatopathologist's subjective judgment, says an expert. Adjunctive genetic tests and morphologic analysis can provide further clues, though neither method is infallible.
Diagnosis of desmoplastic melanoma (DM) often requires immunostaining, as well as the dermatopathologist’s subjective judgment. Similar principles apply for diagnosing other challenging melanocytic lesions, says an expert dermatopathologist who spoke at MauiDerm 2016.
Diagnosing DM

Dr. HighWhitney A. High, M.D., J.D., M.Eng., Associate Professor of Dermatology and Pathology at the University of Colorado School of Medicine, says, "Desmoplastic melanoma is a subcategory of spindle cell melanoma."
Desmoplasia refers to hyperplasia of fibroblasts with increased surrounding fibrous connective tissue. Morphologically, melanomas can either be spindle cell (long, narrow cells) or epithelioid (larger, polygonal cells with more copious cytoplasm).
"Spindle cell melanoma is the umbrella term, and desmoplastic melanoma is a subcategory of spindle cell melanoma." Moreover, he says, DM can be designated as "pure" (comprised of >90% desmoplastic elements), or "mixed" (comprised of <90% desmoplastic elements).
Distinguishing between pure and mixed forms of DM is important because many tertiary institutions do not perform sentinel lymph node (SLN) sampling for pure desmoplastic melanoma, as there is a lower rate of observed metastatic disease in this setting, says Dr. High. "That is why there is interest, on the part of both the dermatopathologist and the clinician, in separating ‘pure’ desmoplastic melanoma from those with ‘mixed’ features."
Because spindle-cell melanoma (without desmoplasia) has a metastatic risk similar to that of epithelioid melanoma, "Many institutions will perform SLN sampling in cases with mixed patterns, assuming the situation is otherwise appropriate for such a procedure," Dr. High says.
Clinically, he adds, DM occurs most frequently on the head and neck, often with an indurated or scar-like appearance, due to its collagenous elements, while spindle cell melanoma, without desmoplasia, favors the trunk and extremities.
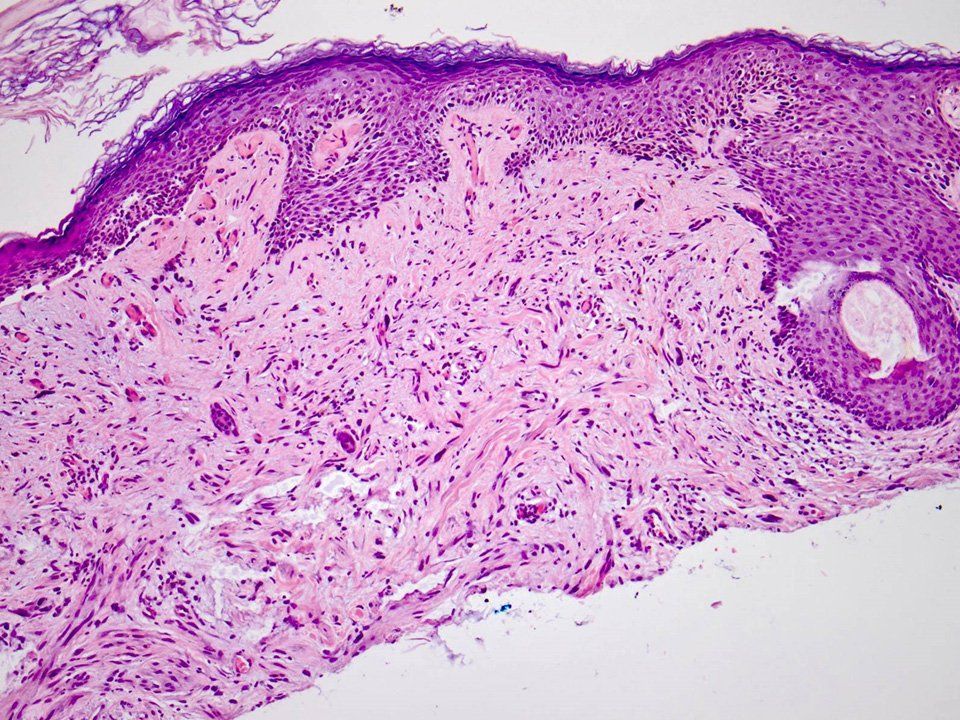
H&E image of a desmoplastic melanoma that was missed in a shave biopsy. Only the melanoma in situ was identified by the board-certified dermatopathologist. The underlying hypercellularity and desmoplasia were mistaken as simple fibrosis.
Photo: Whitney A. High, M.D.Detecting spindle cell melanoma, desmoplastic or otherwise, often requires immunostains, Dr. High says. "Of course, there is no single immunostain that can be used to affirm an assessment of melanoma, per se, but without immunostaining to ascertain the etiologic lineage of the cells, it could be quite difficult to distinguish a spindle cell melanoma from a spindle cell squamous cell carcinoma or an atypical fibroxanthoma (AFX)."
Among immunostains, HMB-45 and Melan A/MART-1 can provide false negative results, particularly in DM, says Dr. High. In contrast, S100 is the most sensitive-although not specific-marker for DM that is in routine use.1 "P75 and SOX10 offer sensitivity levels that are nearly as high as that of S100, but they are not as widely available or employed," he says.
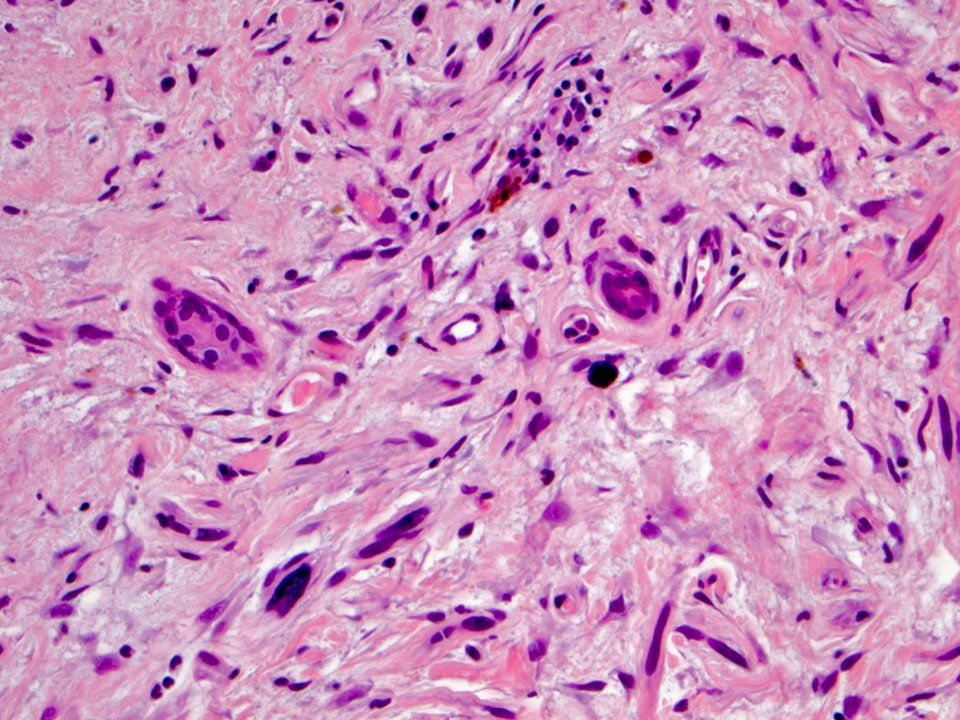
Higher power view of the same case showing the large atypical spindled cells of the melanoma enmeshed in a desmoplastic stroma.
Photo: Whitney A. High, M.D.
Distinguishing among these spindle cell malignancies is important, Dr. High says, because "For a confirmed spindle cell melanoma, one might perform a wider excision, and perhaps even a sentinel lymph node biopsy. For an atypical fibroxanthoma, one might simply settle for conservative but complete removal."
Recently, next-generation gene sequencing of 15 DM samples revealed neurofibromin (NF1) mutations in 93% of DMs. Mutations in this gene, which is associated with neurofibromatosis, are now thought to be common in DM, he says. "Such mutations are also present in a significant number of malignant peripheral nerve sheath tumors, and so, there may be a relationship between DM and malignant peripheral nerve sheath tumors."2
More on melanoma: Moving toward personalized medicine
Next: Other melanocytic neoplasms
Other melanocytic neoplasms
Granted, says Dr. High, assessment of all forms of melanoma is somewhat subjective. There is no laboratory test with 100% sensitivity or 100% specificity for melanoma. "Just as the 'ABCDE' criteria we use in discussing the clinical appearance of atypical nevi are the same criteria we use to discuss the clinical appearance of melanoma, there is significant histologic overlap between desmolastic nevi, atypical nevi, spitzoid nevi and melanoma," he explains.
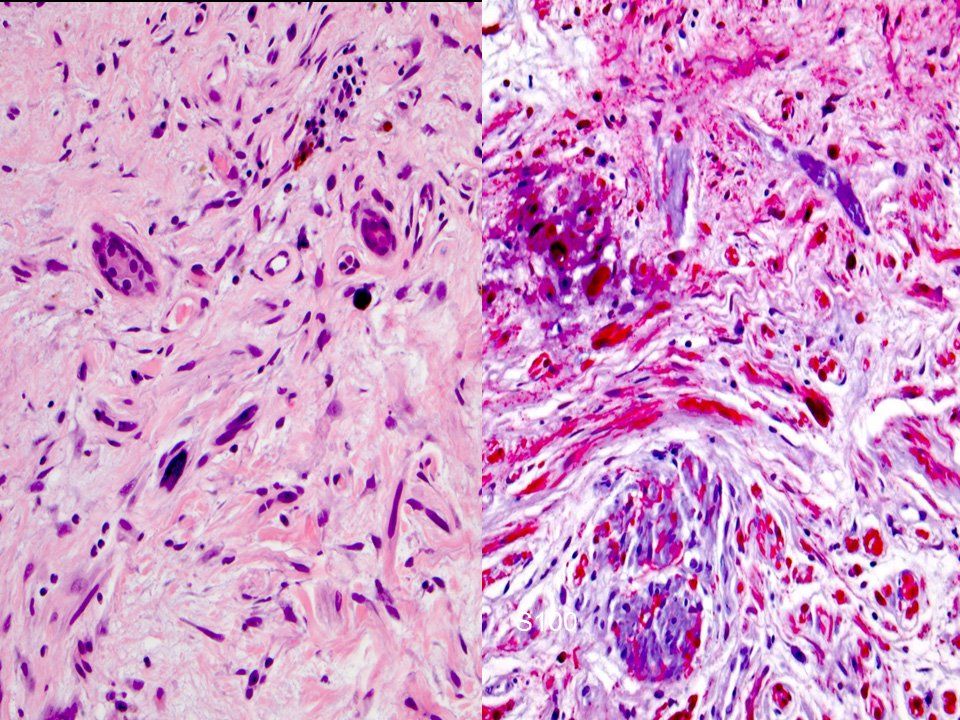
S100 immunostain confirmed strong positivity among the malignant spindled melanocytes of the dermis. Photo: Whitney A. High, M.D.In many respects, diagnosing melanoma is "a black art-short of waiting for biologic 'proof' of malignancy, there is no singular thing I can do to prove something is melanoma, if some other expert says it isn't-pathology reports are called 'histologic opinions' for a reason," Dr. High laments.
Dr. High explains further that "The accurate classification of some difficult melanocytic neoplasms remains a challenge, for all experts." For challenging lesions, he states, "Reasonable differences of opinion with regard to whether something is a frank melanoma, an atypical nevus or an atypical Spitz ‘tumor’ are expected. That is simply the state of medical knowledge in 2016-we need to be honest and forthright with patients about these limitations."
Sometimes immunostains, such as P16, can assist in the assessment of ambiguous melanocytic lesions, he says. "In general, if a difficult melanocytic process expresses P16 in a mosaic pattern, that is a favorable finding, whereas nuclear or cytoplasmic loss of P16 is a more ominous finding, but it is not a 'thumbs-up/thumbs-down' test for melanoma." Other stains used to study problematic melanocytic lesions may include HMB-45 and Ki-67.
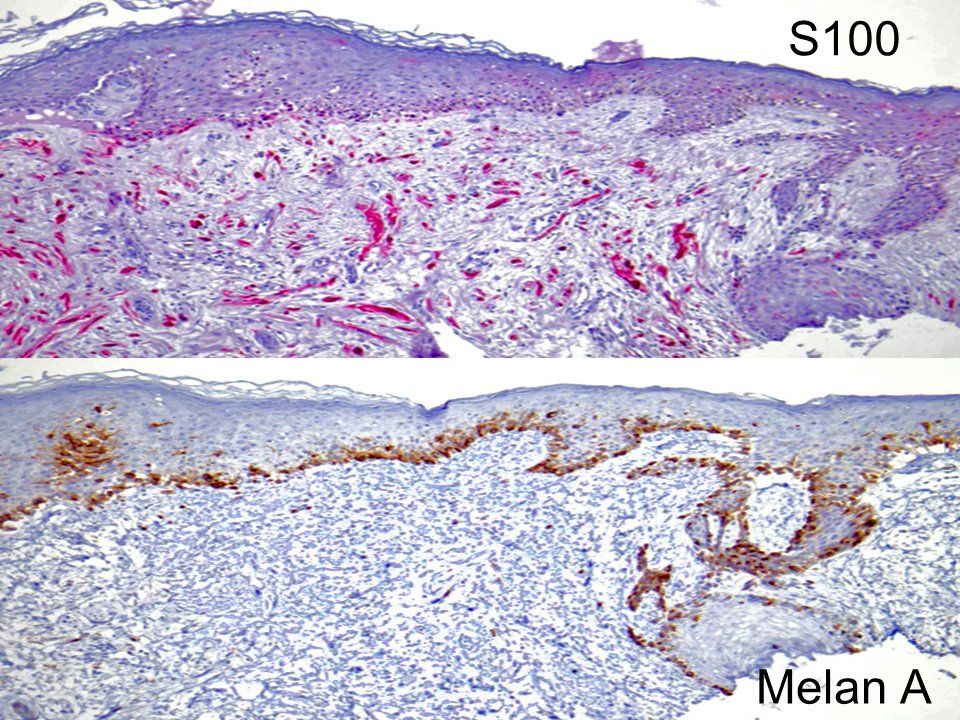
Comparison of the S100 immunostain in desmoplastic melanoma, which affirmatively marks the dermal cells, with the corresponding Melan A/MART1 immunostain, which marks the junctional atypical melanocytes of the melanoma in situ (lentigo maligna) but does not mark the malignant dermal spindled cells of the underlying demsoplastic melanoma.
Photo: Whitney A. High, M.D."I hope that someday, we'll have genetic testing that can give a definitive answer. At present, we have some adjunctive genetic tests-like array-based comparative genomic hybridization (aCGH), fluorescence in situ hybridization (FISH), and gene expression profiling, such as the MyPath Melanoma test (Myriad). But none of these tests has 100% sensitivity and 100% specificity, and hence, there remain some false positives and false negatives with these studies."
Presently, he says, "Dermatopathologists use morphologic analysis, or the assessment of the microscopic appearance and arrangement of cells, as a surrogate marker for the genetic potential of melanocytic lesions. This is no different from 'profiling' flyers at an airport, or literally judging a book by its cover-should we be surprised that on occasion it fails?" Dr. High asks.
He concludes, "There is little doubt that improvements in the objective assessment of melanoma are needed, and with time and a little ingenuity, I believe we will get there."
Of similar interest: Risk factors for melanoma and genetic testing
Disclosures: Dr. High reports no relevant financial interests.
References
1. Weissinger SE, Keil P, Silvers DN, et al. A diagnostic algorithm to distinguish desmoplastic from spindle cell melanoma. Mod Pathol. 2014; 27:524-34.
2. Wiesner T, Kiuru M, Scott SN, et al. NF1 mutations are common in desmoplastic melanoma. Am J Surg Pathol. 2015; 39:1357-62.





