- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
Article
Biopsy process helps pathologist determine accurate diagnosis
Common mistakes related to pediatric biopsies include using the wrong biopsy technique or transfer medium, sending inadequate samples and omitting the child's age.
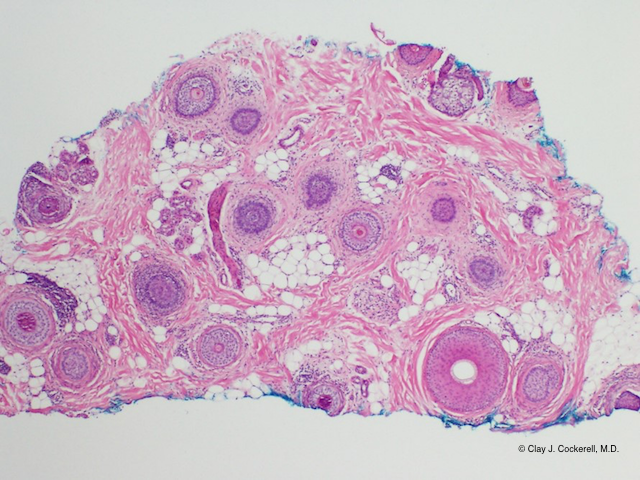
Vertical sectioning allows visualization of an entire follicle, but fewer follicles in number.

Helping a dermatopathologist reach the right diagnosis requires using the right biopsy, labeling and tissue transport techniques.
When a dermatopathologist examines a sample, says Jan Izakovic, M.D., limitations often lie in technical details such as how the specimen was taken, how big it is, and how it's preserved and transported.
Read: Lab, clinical background key in pediatric dermatopathology
"Pathologists would get specimens sent in with a specific question, and they'd say, 'The way you sent it in, I can't do the examination you want done," Dr. Izakovic says. He is a voluntary associate professor of dermatology at the University of Miami and a Basel, Switzerland-based dermatologist who consults in pediatric dermatology at the University Children's Hospital of Basel.
Dallas-based dermatologist and dermatopathologist Clay J. Cockerell, M.D., says that often, "We get samples submitted without any age, and age is important," partly because children are more commonly biopsied for suspected genetic disorders than are adults. Occasionally, "We get shave biopsies of panniculitis or alopecia. These do not sample the area where the pathology is located. We also occasionally get specimens for culture or immunofluorescences submitted in formaldehyde, which renders them both worthless."

Typical non-inflammatory alopecic patches of alopecia areata.


Splitting hairs
If sending hair shafts for analysis, Dr. Cockerell says, "It's important to get the entire shaft with a special device, something like a hemostat with a rubber tip on the end, that allows you to pull the hair shaft from the scalp. If you're going to send hair pulls, make sure that they're done in a way that allows us to look at the base of the hair when it's still inside the scalp, as opposed to just the outer hair shafts themselves."
Read: Central centrifugal cicatricial alopecia
For diagnosing hair loss, says Dr. Cockerell, it's best to take two biopsies (using a sharp punch tube) that the dermatopathologist will prepare into horizontal and vertical sections. To that end, says Dr. Izakovic, the dermatopathologist slices this cylinder of skin in a vertical direction. "But for some hair disorder evaluations, the dermatopathologist should also cut horizontal sections. For that, you must provide at least a 4 mm diameter sample." Punch tubes that give only 1.5 mm in diameter are too small for the pathologist to do both the vertical and horizontal sections, he says.
Also read: Alopecia: New hope for the hopeless
For tinea capitis, which occurs more commonly in children than adults, says Dr. Izakovic, "Make sure the biopsy gets the hair shaft that's affected. If you just get the skin around the hair shaft, it may be artifactually negative."
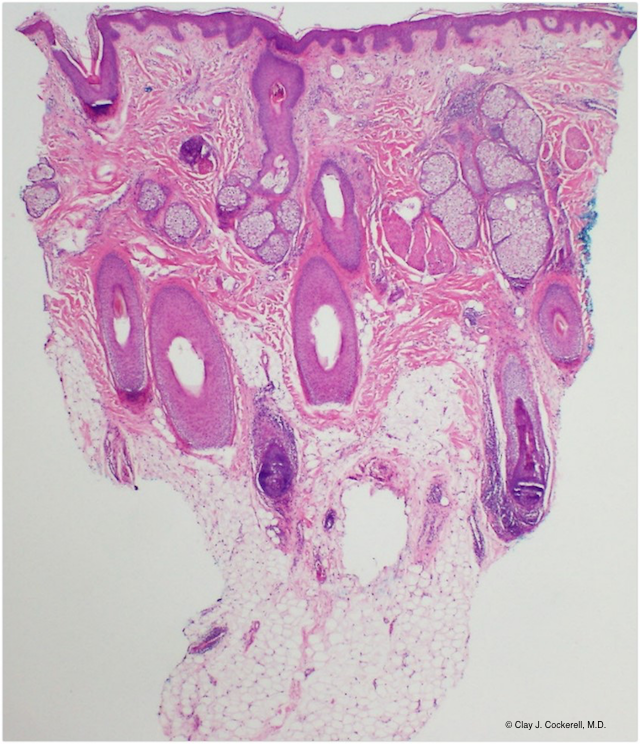
Horizontal sectioning allows visualization of a greater number of hair follicles.

Blistering diseases
For bullous disorders, says Dr. Izakovic, "The pathologist ideally wants to see the transition from normal skin into the start of the blister. So take the biopsy at the blister's edge, having half normal skin, half blister. And it should be thick enough that on the vertical section you can see the transition." Dr. Cockerell says, "The level of the skin in which the blister forms gives us a better idea of the diagnosis. Bullous impetigo or Staphylococcal scalded skin syndrome creates a very superficial blister just beneath the stratum corneum. Pemphigoid occurs beneath the epidermis entirely."
Disclosures: Dr. Cockerell is a speaker and consultant for Myriad Genetics. Dr. Izakovic reports no relevant financial interests.
References
1. Special stains and tests. Http://www.dermnetnz.org/doctors/dermatopathology/stains.html. DermNet New Zealand Trust. 2008. Updated November 2014. Accessed June 3, 2015.
2. Chan LS. Bullous pemphigoid workup. Elston DM (ed). WebMD, LLC. 2011. Http://emedicine.medscape.com/article/1062391-workup. Updated June 12, 2014. Accessed June 3, 2015.





