- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
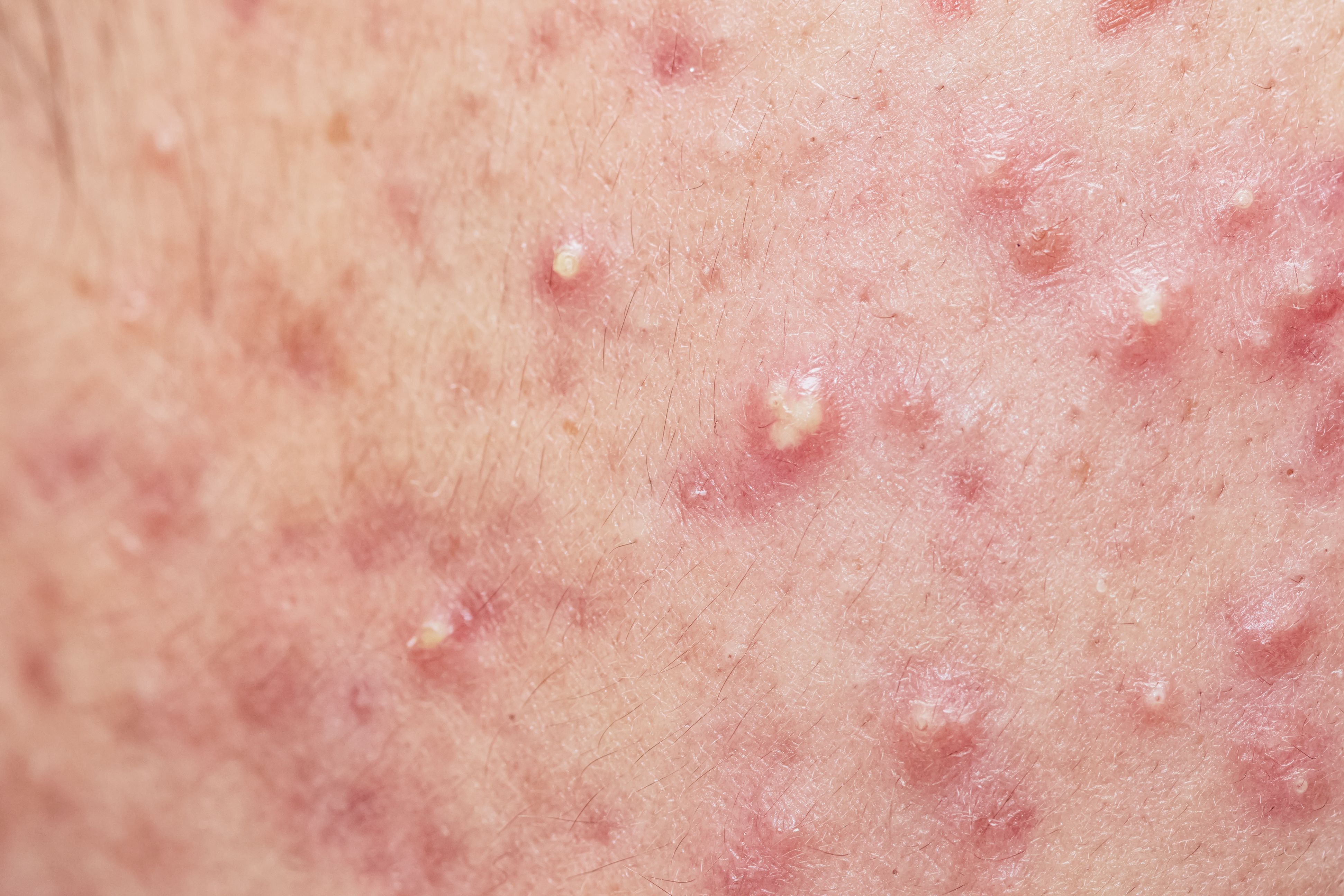
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Article
Avoid antibiotic monotherapy
Author(s):
The cumulative dose of antibiotics prescribed to treat acne can be reduced through adjunctive use of retinoids or benzoyl peroxide.
Curbing the duration of antibiotic prescriptions and prescribing antibiotics in combination with therapies such as benzoyl peroxide or topical retinoids are strategies that dermatologists can implement to respond to the challenge of antibiotic resistance.
READ: 4 helpful references on antibiotic use
Speaking here at a workshop on translating evidence into practical guidelines in acne treatment at the annual meeting of the American Academy of Dermatology (AAD), Jonette Keri, M.D., Ph.D., Associate Professor, University of Miami, Miller School of Medicine and Chief, Dermatology Service, Miami VA Hospital, explained that the Centers for Disease Control in Atlanta is promoting antibiotic stewardship for healthcare professionals because of the growing global crisis of antibiotic resistance.
"This is to ensure that the patient gets the right dose of the right antibiotic at the right time and for the right duration," Dr. Keri said in an interview with Dermatology Times.
In dermatology circles, implementing antibiotic stewardship means avoiding antibiotic monotherapy, whether topical or oral, as well as limiting the use of oral antibiotics, typically not more than three or four months, according to Dr. Keri.
"You don't want to use just one antibiotic, oral or topical," Dr. Keri says. "You want to pair the antibiotic with benzoyl peroxide or a retinoid."
Dr. Keri points to research which recommended benzoyl peroxide should be used in conjunction with topical antibiotics to steer clear of resistance.1
READ: 3 things derms can do now to limit antibiotic use
Not only is there no documented resistance to benzoyl peroxide, the use of benzoyl peroxide avoids the development of antibiotic-resistant P. acnes strains, Dr. Keri explains.
Dr. Keri points to Korean research which concluded that the P. acnes of patients who were exposed to antibiotics, either topical or systemic, to manage acne, demonstrated resistance, while no P. acnes in patients who were not exposed to antibiotics for acne treatment were resistant to antibiotics.2
NEXT: Systemic antibiotics to treat acne
Some of the systemic antibiotics selected to treat acne include doxycycline, minocycline, and tetracycline, noted Dr. Keri, adding that clinicians can look to alternative antibiotics like azithromycin and combined trimethoprim/sulfamethoxazole if patients are intolerant to tetracycline.
READ: Acne pathogenesis
Certainly there are side effects linked to oral antibiotics that are prescribed for acne, Dr. Keri stresses. Doxycycline, for example, is associated with gastrointestinal upset and photosensitivity, while minocycline is associated with blue-grey discoloration of skin, vertigo-like symptoms, and, very rarely, drug-induced lupus. Subantimicrobial-dosing of doxycycline, 20mg orally twice daily, is another therapeutic option for acne patients, Dr. Keri notes. Research has demonstrated that the subantimicrobial dose of doxycycline decreases inflammatory and non-inflammatory acne while producing fewer side effects.3,4
Even with subantimicrobial dosing of antibiotics available, Dr. Keri recommends that patients who are taking oral antibiotics for acne treatment consider adding yogurt to their diet or taking probiotics to replenish their normal gut flora.
Retinoid maintenance is another tactic to decrease reliance on antibiotics and thereby not contribute to the problem of antibiotic resistance. Options include adapalene, tazarotene, or tretinoin. A study published in 2006 found the use of tazarotene gel maintained improvement that was produced after 12 weeks of minocycline 100mg twice daily.5
"You don't have to keep them (patients) on oral antibiotics to keep them clear (and avoid recurrence)," Dr. Keri says. "If you can use a retinoid, you can get away with using less antibiotic therapy."
READ: Acne and anxiety
At the three or four month mark, clinicians should contemplate tapering the dose of antibiotic therapy to treat their patients with acne. In instances where patients are not responding to treatment, clinicians can consider substituting, in their female patients, the long-term use of antibiotics for therapies like oral contraceptives or spironolactone.
In contrast, it was not so long ago that dermatologists prescribed oral antibiotic therapies to their patients with acne without placing a limit on the treatment, Dr. Keri explains. "Three years prescription of antibiotic therapy was not abnormal in the past," Dr. Keri says.
The AAD will be releasing new acne treatment guidelines this year.
Dr. Keri reports no relevant disclosures.
References:
Dreno B, Thiboutot D, Gollnick H, et al. Antibiotic stewardship in dermatology: limiting antibiotic use in acne. Eur J Dermatol. 2014;24(3):330-4.
Moon SH, Roh HS, Kim YH, Kim JE, Ko JY, Ro YS. Antibiotic resistance of microbial strains isolated from Korean acne patients. J Dermatol. 2012;39(10):833-7.
Skidmore R, Kovach R, Walker C, et al. Effects of subantimicrobial-dose doxycycline in the treatment of moderate acne. Arch Dermatol. 2003;139(4):459-64.
Toossi P, Farshchian M, Malekzad F, Mohtasham N, Kimyai-asadi A. Subantimicrobial-dose doxycycline in the treatment of moderate facial acne. J Drugs Dermatol. 2008;7(12):1149-52.
Leyden J, Thiboutot DM, Shalita AR, et al. Comparison of tazarotene and minocycline maintenance therapies in acne vulgaris: a multicenter, double-blind, randomized, parallel-group study. Arch Dermatol. 2006;142(5):605-12.