- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Publication
Article
Dermatology Times
Aggressive, early treatment may prevent acne scars
Author(s):
Treating all acne early with a topical retinoid and an antibiotic can help patients avoid scarring and its psychosocial consequences, experts say. The aggressive approach also may help stave off medicolegal concerns, they add.
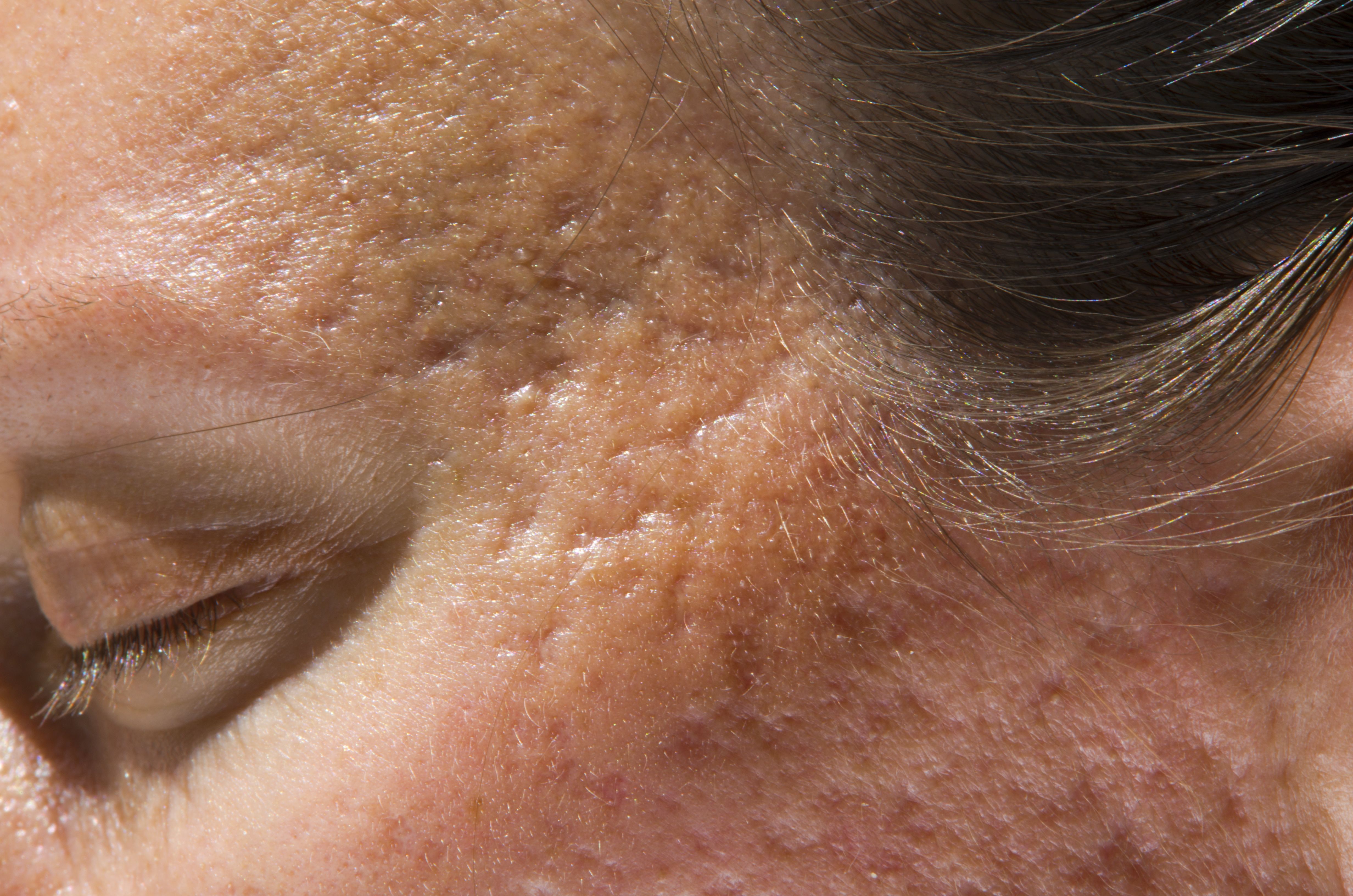
"I suggest you haul out your magnifying glass and look carefully for any signs of scarring. That's important for medical as well as medicolegal reasons," says Hilary Baldwin, M.D., Acne Treatment and Research Center, Morristown, N.J. (©BudimirJevtic - stock.adobe.com)
Dr. Baldwin

Dr. Tanghetti

Treating all acne early with a topical retinoid and an antibiotic can help patients avoid scarring and its psychosocial consequences, experts say. The aggressive approach also may help stave off medicolegal concerns, they add.
RELATED: Studies support microneedling efficacy for acne scarring
Medical dermatology can address subtle scars, says Hilary Baldwin, M.D., director of the Acne Treatment and Research Center in Morristown, N.J. In this regard, the OSCAR study showed that benzoyl peroxide plus adapalene improved scars approximately 30% at six months versus the untreated side in a split-face study.1
"Treatment not only prevented the development of new scars," says Dr. Baldwin, "but it also eradicated some of the pre-existing scars."
Mechanistically, she says, the retinoid adapalene is more likely than benzoyl peroxide to explain these effects. Tretinoin has shown similar effects in reducing2 and preventing scars.3
A recent study by Loss et al. showing that adapalene 0.3% gel alone achieved significant improvements in moderate-to-severe acne scarring of 19.3 years' mean duration4 is another important piece of the puzzle, says Emil Tanghetti, M.D. He is director of the Center for Dermatology and Laser Surgery in Sacramento, Calif.
Together, he says, Loss et al. and OSCAR show that treating early and effectively can stop acne and scarring and possibly improve some pre-existing scars. "With lasers and lights, you can go so far. But having an extra tool that can work in concert makes eminent sense," he says.
The new research allows him to tell patients with active acne, "we're not only going to treat your acne, but you're also going to improve the scars, which is a big deal." Furthermore, says Dr. Tanghetti, patients with existing scars can afford and use adapalene gel on their own.
RELATED: Why does acne leave a scar?
Even mild acne can scar. An international survey of dermatologists and health records revealed that the proportion of patients with mild acne who experienced scarring ranged from 22 to 28%.5 Accordingly, Dr. Baldwin says that when first seeing a patient, check carefully for early signs of scarring.
"I don't think we look carefully enough at our patients with acne, because we don't 'need' to. They walk in the door, and it takes five seconds to know how, other things being equal, you would treat that patient," she says. The rest of the visit is spent ensuring that the treatment plan suits the patient.
"I suggest you haul out your magnifying glass and look carefully for any signs of scarring. That's important for medical as well as medicolegal reasons," adds Dr. Baldwin.
Medically, she explains, pointing out early signs of scarring to patients and parents supports one's recommendation for aggressive therapy. "For medicolegal reasons, document the presence of scars at the very beginning, before you start treatment, because we tend to get blamed for things later on."
Along with acne severity, scarring risk factors include male gender, high body mass index (BMI) and a family history of acne. "The BMI link is not strong enough to say, 'If you just lost some weight, your acne would improve.' And you can't change your family or gender. So the only thing you can do is to make sure that you're adequately treated," Dr. Baldwin says.
In the recent past, she says, dermatologists have begun recognizing that the longer they wait to treat acne well, the more likely patients will scar.5,6,7
RELATED: A place for deep peels in acne scar treatment
"And this seems to be most true in the first three years of acne development," she says. Parents sometimes wait to treat acne until children are older because they fear giving young girls oral contraceptives, or they fear using isotretinoin altogether.
"The longer you wait, the more likely you are to create scars,” says Dr. Baldwin, However, she says, many dermatologists have not yet embraced this philosophy. Concerned about irritation, they start with other drugs and add topical retinoids later.
"The data suggest that we ought to be treating with topical retinoids from the very beginning in every patient with acne," she says.
Tactics to reduce retinoid irritation include every-other-day application and moisturizing first. "And then just grin and bear it. After the first two weeks, it generally doesn't irritate anymore," Dr. Baldwin adds.
Acne scars also can cause emotional scars, says Dr. Baldwin. When children say that peers stare at or talk about their acne and scars, she says, patients and physicians often downplay these concerns.
"The tendency is to say, 'Oh sweetie, that's not true. Maybe they're talking about something else,'" she notes. However, research shows that people indeed judge others with acne scars to be less attractive, confident, happy, healthy and successful.8
RELATED: 10 Treatment options for acne scarring
Still, Dr. Tanghetti says that he finds quality-of-life studies difficult to put into perspective.
"I always want to do the best I can for patients. I let the patient be the judge of what to treat. Who am I to judge how acne affects someone?"
Provided the acne is under control (and the patient does not have body dysmorphic disorder), he says, mild-to-moderate scars are often highly amenable to topical and device therapy. "We can get outstanding results with those,” he says. “The deeper, more severe scars are always going to be a bigger challenge."
Device-based treatments
In treating moderate-to-severe scars with devices, says Dr. Tanghetti, practitioners used to swing for "home runs" using fully ablative CO2, aggressive fractional CO2 and aggressive nonablative fractional processes.
"But we're seeing now that patients want to preserve their activities. So rather than trying to do it in one or two treatments, we're doing it in three to five, with less aggressive settings and less downtime, and getting modest to good results," he says.
He avoids lasers and lights with keloids because overaggressive treatment can worsen them. "We treat primarily the boxcars, ice picks and smaller pock marks," he adds. Dr. Tanghetti treats these scar types similarly because patients usually have a combination of lesions. He typically avoids subcision and fillers until seeing how laser therapy, and possibly radiofrequency microneedling (RFMN), perform.
RELATED: The psychosocial burden of acne
"There's an incredible number of devices available for acne scars," Dr. Tanghetti says. Rather than creating days to weeks of downtime with aggressive resurfacing, he adds, there are ways to use devices such as the SmartXide Tetra CO2 (DEKA), which has high-pulse, low-wattage settings that ablate the epidermis and cause minor dermal wounding.
"There's virtually no downtime,” Dr. Tanghetti says, “We even do it without anesthesia."
After treatment, patients can apply moisturizer and light makeup and return to work immediately.
Combining lasers with microneedling allows deeper treatments. If combining laser treatments with RFMN, Dr. Tanghetti suggests applying topical anesthetic before microneedling, followed by the laser.
Dr. Tanghetti also uses a 755 nm fractional picosecond laser in various skin types.
"We've found that with the lens arrays that are used with picosecond technology, I can even treat very dark African-American skin and get some improvement of acne scars with relatively superficial treatment.” Epidermal injuries promote release of cytokines that cause rejuvenation and scar remodeling over time, he explains.
RELATED: A paradigm shift in the treatment of acne
Based on the success of adapalene with and without benzoyl peroxide, he adds, many developers are exploring whether other retinoids can achieve similar effects.
"The leading contenders would be tretinoin and tazarotene. Altreno (tretinoin, Ortho Dermatologics) would be a great fit because it's very tolerable and spreadable," he says.
Additionally, Ortho Dermatologics has submitted for FDA approval its tazarotene lotion (IDP-123) that uses the same polymeric mesh vehicle, which Dr. Tanghetti says includes humectants and emollients that dramatically boost tolerability.
Disclosures:
Dr. Tanghetti is a consultant for Cynosure, DEKA, Quanta, Cartessa and Aesthetics Biomedical but owns no stock in these companies. He holds an ownership interest in a laser under development for active acne. Dr. Baldwin is a consultant and/or researcher for Galderma and Ortho Dermatologics.
References:
1. Dréno B, Bissonnette R, Gagné-Henley A, et al. Am J Clin Dermatol. 2018;19:275-286.
2. Schmidt JB, Donath P, Hannes J, Perl S, Neumayer R, Reiner A. Int J Dermatol. 1999;38:149-153.
3. Mandy SH. J Am Acad Dermatol. 1986;15(4 Pt 2):878-879, 888-889.
4. Loss MJ, Leung S, Chien A, Kerrouche N, Fischer AH, Kang S. Dermatol Ther (Heidelb). 2018;8.245-257.
5. Dréno B, Layton A, Bettoli V, Torres Lozada V, Kang S. 23rd EADV Congress; October 8-12, 2014; Amsterdam.
6. Layton AM, Henderson CA, Cunliffe WJ. Clin Exp Dermatol. 1994;19:303-308.
7. Tan JK, Tang J, Fung K, et al. J Cutan Med Surg. 2010;14:156-160.
8. Dréno B, Tan J, Kang S, et al. Dermatol Ther (Heidelb). 2016;6:207-218.






